SAMHSA released the 2019 National Survey on Drug Use and Health (NSDUH) Annual National Report this week.
One of the sections that’s gotten a lot of attention on Twitter is Substance Use Treatment in the Past Year.
The item that seems to have received the most attention is Reasons for Not Receiving Substance Use Treatment.
In particular, that the most common for reason for “not receiving substance use treatment among people aged 12 or older with a past year Substance Use Disorder (SUD) who did not receive treatment at a specialty facility and perceived a need for treatment were as follows: not being ready to stop using (39.9 percent)” [emphasis mine]
The concern is that the emphasizing this as the top reason for not seeking treatment reinforces myths and stigma about people with substance use problems.
Let’s break it down
“not receiving substance use treatment” – This finding is based on people who did not receive treatment. People who did receive treatment are not included. So, this does not represent people with an SUD, just people with an SUD who did not receive treatment in the past year.
“among people aged 12 or older” – This finding includes a very large age range. Let’s look at the sub-ranges included:
- Among adolescents aged 12 to 17 in 2019, 4.6 percent (or 1.1 million people) needed substance use treatment in the past year.
- Among young adults aged 18 to 25 in 2019, 14.4 percent (or 4.8 million people) needed substance use treatment in the past year.
- Among adults aged 26 or older in 2019, 7.2 percent (or 15.6 million people) needed substance use treatment in the past year.
So, respondents aged 12 to 25 make up 37.5% of those included in this statistic. A couple of things come to mind about this group. First, we would expect lower levels of readiness to change among this group. In the case of addiction (the most severe form of substance use problems) the time between the first use and the first help-seeking is typically 4 to 5 years. We also know that earlier onset typically results in longer addiction careers. Second, we know that more than half of people under the age of 26 with alcohol dependence will “mature out” or experience “spontaneous recovery” without treatment.
“with a past year SUD” – This invites questions about how SUD is defined.
The report says the following, “The SUD questions classify people as having an SUD in the past 12 months based on criteria specified in the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV).”
The DSM-IV had 2 categories of SUDs–Abuse and Dependence. The diagnosis is substance-specific (e.g. – Cannabis Abuse, Alcohol Abuse, Opioid Abuse, etc.) and Abuse is the less severe of the 2 categories of disorders. The diagnostic criteria are as follows:
A maladaptive pattern of substance use leading to clinically significant impairment or distress, as manifested by one (or more) of the following, occurring within a 12-month period:
- Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home (e.g., repeated absences or poor work performance related to substance use; substance-related absences, suspensions, or expulsions from school; neglect of children or household)
- Recurrent substance use in situations in which it is physically hazardous (e.g., driving an automobile or operating machinery when impaired by substance use)
- Recurrent substance-related legal problems (e.g., arrests for substance-related disorderly conduct)
- Continued substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance (e.g., arguments with spouse about consequences of intoxication, physical fights)
One of the criticisms of DSM IV Abuse what that the threshold was too low for categorizing it as a disorder. For example, a college student who gets convicted of Minor in Possession of alcohol and is put on probation, and later discovered to be drinking again would meet diagnostic criteria for Alcohol Abuse.
The report does not break down the prevalence of Abuse vs. Dependence among the respondents.
It’s also noteworthy that most people meeting criteria for DSM Abuse will not need to abstain to resolve their problem–most of them will moderate their substance use without any help. The report also points out that many people who meet criteria for dependence will not need treatment and many of them will also be able to moderate.
I believe that the combining of these people with others who have chronic and severe substance use problems into the category Substance Use Disorders renders the category meaningless. This is an unpopular view in advocacy circles.
“and perceived a need for treatment” – This invited questions about how perceived need was determined. The NSDUH used the following question, “During the past 12 months, did you need treatment or counseling for your alcohol or drug use?”
I imagine that asking people if they needed counseling at some time in the past year for alcohol or drug use significantly lowers the threshold for inclusion into the group with a “perceived need” for treatment.
“not being ready to stop using” – The concerns raised in multiple tweets by multiple advocates centers on 40% of people with an SUD and a perceived need for counseling or treatment not receiving treatment because they reported “not being ready to stop using.” [emphasis mine]
That response indicates an assumption that counseling/treatment requires abstinence from use of (at least) the substance in question. As mentioned above, abstinence is probably not a necessary or appropriate goal for most people meeting criteria for DSM IV Abuse and many people meeting criteria for Dependence.
So … this option could capture any respondent with low problem severity, high insight, and ambivalence about abstinence.
What’s the problem?
Does this finding misrepresent people with SUDs?
Does it reinforce stigma?
I don’t know whether it reinforces stigma and I can’t say for sure whether it misrepresents people with SUDs. However, this highlights a problem I’ve posted about several times–SUDs is not a useful category. (Bill Stauffer also posted about it here.)
I’ll go further–the use of this category harms people with addiction and may increase stigma towards them.
- This category results in the conflation of people with lower severity problems who “mature out” and people who have chronic, severe, and treatment resistant addiction.
- This category results in arguments that moderation is an appropriate goal for the category. It also results in arguments that abstinence is the only appropriate goal for the category.
- This category too often turns “maturing out” into an argument against the need for treatment.
- This category contributes to the erosion of the conceptual boundaries of addiction and recovery.
Overshadowing stigma?
Among the complaints that this reinforced stigma was another complaint that the grouping of responses obscured stigma, which should have been listed as the largest reason for not seeking treatment among people who perceived a need for treatment.
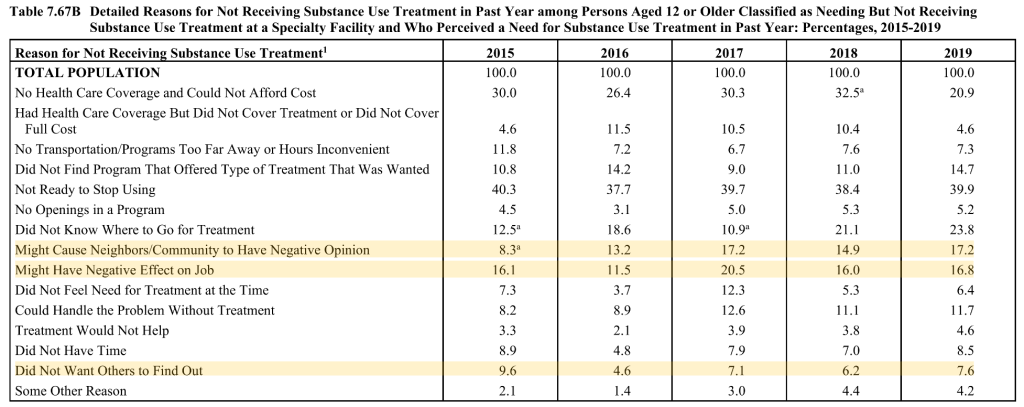
This argument is based on 3 reasons that seek to quantify stigma adding up to 41.6%.
Stigma is a significant barrier to treatment, but I suspect that 41.6% overstates the role of stigma.
- It seems safe to assume that 100% of “might cause neighbors/community to have negative opinion” selections represent stigma.
- “Did not want others to find out” seems a little less clear. A lot of people don’t want others to know anything about their health or personal life. However, that desire for privacy typically doesn’t prevent people from seeking treatment. So, it’s probably safe to assume that most of these responses represent stigma.
- “Might have a negative effect on job” seems much less clear. This could represent fear of stigmatization or it could represent concern about required recurring appointments that might interfere with work attendance.
- Finally, respondents were able to select more than one reason. (The responses total 193.4%.) It’s probably safe to assume there’s some overlap with these three responses.
None of this suggests that stigma isn’t a barrier to treatment or that it’s unimportant. (This blog has 188 posts with the word “stigma” going back to 2006.) I just believe the facts are compelling enough without having to inflate the numbers of people suffering or recovering. I also worry that stigma is so frequently invoked as an explanation for nearly every “problem” in the field that we are eroding the meaning and impact of the term. I believe that doing so will eventually erode our credibility. (I put problem in quotes because many problems in the field are in the eye of the beholder.)
I believe the problem with the reports about the NHDUH is not the the way it’s presented, but the use of this category that includes people making unhealthy decisions about their alcohol and other drug consumption and people with chronic and severe forms of the disease addiction. Imagine a report on “respiratory disorders” that treats common colds and lung cancers as belonging to a single category.