 Recovery is a fresh start through which people aim to find joy and purpose in everyday life without the need for substances. Without substances to turn to and help keep their mind off difficult times in life, people need something else to help ground them and keep them pushing forward, helping and caring for others around them in need. This is where spirituality comes into play. No matter your personal beliefs, spirituality is something every single person is capable of practicing, and doing so is a strong motivator to continue maintaining your sobriety.
Recovery is a fresh start through which people aim to find joy and purpose in everyday life without the need for substances. Without substances to turn to and help keep their mind off difficult times in life, people need something else to help ground them and keep them pushing forward, helping and caring for others around them in need. This is where spirituality comes into play. No matter your personal beliefs, spirituality is something every single person is capable of practicing, and doing so is a strong motivator to continue maintaining your sobriety.
What’s the difference between spirituality and religion?
- A common misunderstanding of the 12 Step Program is that it is grounded in religion and focused on serving one God. Most people tend to conflate spirituality with religion, and in doing so, shy away from finding a higher power because they associate it with religious practices that they may or may not be comfortable with. Spirituality and religion are two very different things – you don’t need to be religious at all to find liberation and comfort in spirituality.
- Religion is made up of rituals and prayers, and each religion has a set of doctrines or beliefs that they adhere to. There may also be specific conditions for membership, as well as an air of righteousness or judgement upon other religious groups or non-religious people. There are specific guidelines for communicating with religious gods.
- Spirituality, on the other hand, is anything that you personally believe in that gives you freedom and peace of mind. Spirituality is about remaining humble and grateful for life, accepting your powerlessness, and staying connected to a higher power – something bigger than yourself that serves as your driving force for making it through each day and meeting your needs. Your higher power can be whatever you desire – a god of your choosing, or a force of the universe, like nature. Your higher power can even be something as abstract as an idea. How you communicate with your higher power is up to you. There is no ‘right way’ to be spiritual.
Why is spirituality important for recovery?
- The human spirit is wired for connection. Without that connection, we have an empty void that we must fill. At that point, addiction issues begin to arise, as people lack that spiritual connection with a higher power and can potentially turn to drugs and alcohol to fill the void.
- Spirituality gives you a sense of identity and purpose. In active addiction, drugs and alcohol made it difficult to understand what your identity and purpose were – substances served to keep your mind off difficult topics like self-acceptance. An addict is living in ‘unreality,’ completely separated from their true thoughts, feelings, and relationships, and dealing with fear and isolation. This is often referred to as the ‘bottom,’ and is where many people become motivated by a need for change to finally reach out to a higher power and make that spiritual connection.
- Admitting you are powerless to your addiction is Step 1. The humility it takes to come to terms with that is only possible through spirituality. You have to find comfort and motivation in a higher power bigger than yourself, and look to that higher power for guidance, in order to be able to love, care for, and connect with others in your life.
- Embracing spirituality and finding your higher power opens up your life to spirit-nourishing practices such as meditation, mindfulness, reading, exercise, or anything else that makes you feel good and helps you grow. Spirituality pushes you out of your comfort zone and encourages you to dedicate time and effort towards bettering yourself. When you focus on improving your life and helping those around you, you’re much more likely to remain sober.
***
For more information, resources, and encouragement, “like” the Fellowship Hall Facebook page and follow us on Instagram at @FellowshipHallNC.
About Fellowship Hall
For 50 years, Fellowship Hall has been saving lives. We are a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.
This is the first post in a series within which I will provide an overview and history of the Recovery Alliance Initiative.
Here’s the Alliance website in case you would like to check that out.
The Recovery Alliance Initiative began as an idea in 2013.
What started as an idea developed into a structured method of bringing together divergent sectors within our field, and guiding them in:
- beginning collaboration across their differing systems
- developing awareness of needs for our field that remaining siloed would not reveal
- forming working groups to take on those needed improvements as formal change projects
- and simple cross-fertilization across their sectors
And in all of this, we work at keeping the effort centered in the sake of the individual person being served.
I’ve presented a good amount of this information at a variety of national, state, county, and other gatherings over the years. And I’ve published materials related to this effort in various forms. But this is the first time and place I’ll be directly covering the whole topic, across the entirety of the project’s lifespan, in writing. The last post in the series will include the list of references for this series and suggested readings.
Origin
The way the Alliance started is a story that to me personally is rather funny.
Tom Edwards, whom I know quite well and has worked in our field for decades, said to me on a phone call late one afternoon in 2013, “Collegiate recovery programs, and professional monitoring organizations – what do they have in common? Tell me why to put them in the room together.”
I really wanted to take time to consider that question and so I asked him for “…permission to think” before I answered. He granted me that permission.
Two weeks later I called Tom and said, “Hey Tom, do you remember that question you asked me?” He said he had no idea what I was referring to. I reminded him of the question he had asked and that he gave me “…permission to think.” He said, “Oh, yeah.” I said, “They’re the same person.”
He stated politely that it seemed I misunderstood his question. He clarified his question and again asked me what the different people served in those two systems had in common.
I put my reply to him this way: “Tom, they’re the same person. Someone who is a licensed professional today was a student yesterday. It’s the same person.”
He totally got it.
The subsequent conversation we had sparked a focused (and at times rather laborious and intense) collaboration between us that has lasted from that moment to the present day. (As an aside it’s worth pointing out that Tom and I are very different from each other in many ways, the least of which is not the fact that he is not a clinician.)
Based on the idea that continuity could exist between collegiate recovery programs and professional monitoring organizations, we planned to facilitate a gathering of leaders from those sectors.
In 2014 we invited some leaders from those two sectors, as well as some others that work with those patients, to meet at a gathering Tom and I would facilitate.
For this first gathering we focused on the national level. By “national level” I mean two things.
- We invited some people that functioned at the national level within their sectors.
- And we also invited leaders from those sectors that worked locally or regionally but were at the national-level in their knowledge and skill.
So that year we began to hold national-level summit meetings helping those two systems to meet and interact.
During our process of structuring and facilitating those early gatherings, Tom and I noticed key cultural and practical differences between the collegiate recovery and professional monitoring systems. While we facilitated the attendees through our process the differences between these systems emerged and became quite clear. This became rather awkward for us and for some of the attendees. And the process Tom and I were facilitating at times became somewhat difficult for us to manage. Tom and I were less prepared than we thought we needed to be.
I’ll say more a little later about some of the major differences between those systems that emerged during that process.
Tom and I learned a lot of things on a lot of levels from our facilitation of those early Summit meetings. Part of what we learned included how we would go about things differently.
Largely in response to the differences that emerged, I made and attempt to learn and took on a fair amount of reading. Within the next year or two I read a rather large amount of literature examining the theory, method, evaluation, and effectiveness of those two very different systems. I also read related book chapters, monographs, peer reviewed review articles, and so on.
Next, having done more than a little reading, I started to do some professional writing on the topic. In that process I was helped in my clarity and focus by another challenge Tom gave me. He said, “People like visuals. Turn your main idea into a visual diagram.”
For me that was hard. I’m often a visual thinker, but not so for this. All I could come up with at the time was one simple visual model that seemed unimpressive to me. I sketched it and gave that drawing to someone who does visual layouts for us. I showed the final art work to Tom. It was simple enough that he liked it. I was surprised. Here it is.
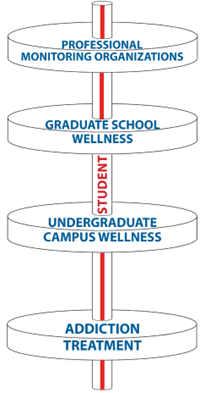
The image above includes a number of ideas. Here are a few of the main ones.
- The person served is central to our purpose.
- Relative to our systems, the person has a long timeline (upward) of their personal life.
- The top of the system is open, connoting in-flow and a relatively green ecology.
- I wanted to show the potential of long-term support being available over time.
- I also wanted to show the caution or problem of unnecessary gaps.
During our Summit meeting we had the sector leaders describe their philosophies and operational methods to each other. The cultural divide between these two kinds of systems was shown to be very wide. As the different sectors shared, the content at times was difficult for the attendees from the other system to receive. And for Tom and me the process of promoting mutual education and formation of support across these systems was at times difficult to facilitate. The divisions were quite real.
I wrote up the essence of my thinking and published an article in 2015. If you’re reading this blog post, I would encourage you to read that article (Coon, 2015).
Part of what I covered in that article were the cultural and practical differences Tom and I came to discover that exist between those two systems. For example, I described that the emphases of accountability and advocacy were generally reversed in their order of priority between those two systems.
- For collegiate recovery programs (CRP’s) advocacy is central, and the program can also include accountability secondarily, as needed.
- But in a professional monitoring organization (PMO) accountability is relatively central, and advocacy can eventually come about as a result.
In my next post in this series, I’ll describe the early evolution of the Alliance. That will include a description of how we clarified and improved our method at bringing numerous and disparate specialty sectors in our field together. And it will cover how we went about helping those sectors form mutual and collective collaboration and advocacy.

Recovery journeys are dynamic, take time and for those who receive treatment, may need several episodes. For some, residential rehab is part of the journey, just as harm reduction interventions can also be part of the journey. However, residential rehabilitation is a complex intervention and complex interventions are difficult to study.
In Scotland, the government is making rehab easier to access and growing the number of beds. This development is not without its critics. Some feel the resource needs to ‘follow the evidence’ – in other words into harm reduction and MAT interventions. This all-the-eggs-in-one-basket position would reinforce the rigid barriers that make rehab the domain of the wealthy or the lucky.
‘Follow the evidence’ in this context is a refrain that implies that there is no evidence that rehab works to help people achieve their goals and improve their quality of life. That is simply not true. Last month saw the publication of a literature review on residential rehab by Scottish Government researchers. It’s a thorough piece of work. This summary of the research evidence provides verification that “that residential rehabilitation is associated with improvements across a variety of outcomes relating to substance use, health and quality of life”.
Rehab is linked to improvements in mental health, offending, social engagement, employment, reduction in substance use and abstinence. There is little research that compares rehab with other treatments delivered in the community, but where there is, the evidence suggests that “residential treatment produces more positive outcomes in relation to substance use than other treatment modalities.” The review also suggests that rehab can be more cost-effective over time than other treatments.
The report also highlights problems and gaps in the evidence base. What happens within the walls of rehabs is diverse and the models and delivery vary, so when we talk of rehab we are not talking about something uniform. We need to gain an understanding about the most effective interventions. Research suggests, for instance, that integrating mental health care into rehab treatment is associated with better outcomes.
The Scottish Government’s literature review highlights gaps that need to be plugged. I think it’s fair to say that there are no queues of Scottish academics curling round the block – researchers chomping at the bit to get their teeth into studies on the place of rehab in treatment and recovery. That we have unanswered questions is not a surprise. Further, it’s important for us to face up to the fact that rehab is not necessarily without risks to individuals, particularly for those with opioid dependence. Those need to be faced square on.
In terms of research, residential rehab, mutual aid, lived experience recovery organisations (LEROs) and community recovery programmes have been largely neglected.
Indeed, the perception of such risks may be one of the main reasons for resistance to rehab as an intervention. We don’t know if those going to rehab in Scotland have higher mortality than in other kinds of treatment, but there is evidence from elsewhere that this could be the case. However, it is plausible that people with higher problem severity (and higher risk of death as a result) end up in rehab. The mortality rate in intensive care units is higher than in general wards, but we don’t stop people going to intensive care because of that.
We also need to be aware that there are mitigations that can be employed to reduce risks. These may include things like comprehensive aftercare, re-titration of those who want to leave treatment early and rapid re-entry into prescribing services if individuals return to use.
Recovery housing, take-home naloxone, overdose prevention, assertive referral into recovery community resources, outreach and recovery check-ups may also reduce risks. Standards could be developed to encourage the adoption of such practices. The impact of these have not been tested in research, but they could be.
I don’t believe it is in the interests of those individuals (and their families) who struggle with dependence on substances for us to maintain treatment turf wars. We can have harm reduction and recovery. We can have MAT and abstinence. We can have outpatient treatment and residential rehab. Whatever we have, it needs to be plugged into supports across housing, criminal justice, benefits, education, training and employability and health. A joined-up, comprehensive treatment system with strong links between its component parts will serve individuals best.
We don’t need to say one thing is better than another, but we do need choice and through shared decision making we can try to help patients align themselves to a treatment option that helps them meet their goals. And we need to be humble too. Evidence suggests that over a lifetime, most people resolve their problematic use of substances. When they look back, they may be grateful for the part that treatment played in their recovery, but it is likely that it will be only one of many factors that helped.
For the moment though, we can certainly challenge the voices that say ‘there’s no evidence that rehab works’, for there is ample evidence that it does. I’m not unrealistic about this though. As I’ve been writing, I have been mulling over the wisdom of Ahmed Kathrada’s observation: ‘the hardest thing to open is a closed mind’. That shouldn’t stop us trying.
Continue the discussion on Twitter @DocDavidM

Michael Werner has been with SMART since the beginning, though not in recovery himself. His motivation, as a facilitator, comes from seeing people transform their lives. If he’s learned anything, it’s that people are resilient and to never give up on them.
Learn more about becoming a SMART volunteer
25 in 25 Volunteer Spotlight: Michael Werner
Subscribe to the SMART Recovery YouTube Channel
Video storytelling is a powerful tool in recovery, and we are proud to share our SMART Recovery content free-of-charge, available anywhere, on any device. Our videos hope to inform, entertain, and inspire anyone in the recovery community.
Subscribe to our YouTube channel and be notified every time we release a new video.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
| Here at NADCP, we’re humbled and grateful for you, the treatment court field. This May has been a beautiful tribute to the lives you’ve helped save, families you’ve kept together or reunited, and paths you’ve carved out of the legal system and into long-term recovery for thousands of Americans. Thank you. NADCP is also grateful to our federal partners, who took to social media to support your work all month long. And we saw many state proclamations and graduation speeches by your state’s leaders – from governors to members of Congress, they showed up to support treatment courts and the graduates. Plus, we’ve been blown away the artistic talents of your participants and alumni as they’ve entered our Art of Recovery contest. The winners will be announced soon; be sure to stop by and take in the gallery at RISE22! |
| Here are just a few of the incredible stories and images you’ve sent us and that have headlined the news over the last 10 days. |
| AZ treatment court hits two huge milestones |
| DWI Academy Court stands out |
| Supporting veterans in Albuquerque |
| Annual Sacramento river cleanup event a success |
| 5K race celebrates multiple treatment courts |
| First graduation in rural Louisiana |
The post National Drug Court Month Week 4 appeared first on NADCP.org.
| What else can we say but THANK YOU for your tireless work promoting and educating the public about your programs! The commencement ceremonies, proclamations, social media posts, and graduate success stories are what make National Drug Court Month great. Please continue to send us your artwork for our Art of Recovery contest! Here’s a small portion of all the amazing activity from week three! |
| U.S. Senator John Boozman encourages Arkansans |
| National mentor court receives recognition |
| Detroit treatment courts graduate two dozen |
| Veterans Affairs blog tells a recovery story |
| Austin DWI court holds first in-person ceremony |
| Family treatment court sees lives changed and families reunited |
| Headline of the week: “West Virginia adult drug treatment programs provide success that could last generations” |
The post National Drug Court Month Week 3 appeared first on NADCP.org.
“[Recovery] changed my life… it was the best thing I ever did. My big worry when I got sober was, ‘I’m not going to have fun anymore.’ Someone gets married and I’m not gonna have a drink? Guess what – I didn’t have any of that, and it’s been awesome.”
Actor, producer, and director Rob Lowe discusses what he enjoys the most about being in recovery after 30 years of sobriety – and offers his best advice to those struggling with addiction, as well as the family members around them.
***
For more information, resources, and encouragement, “like” the Fellowship Hall Facebook page and follow us on Instagram at @FellowshipHallNC.
About Fellowship Hall
For 50 years, Fellowship Hall has been saving lives. We are a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.
Guest blog by Jeffry Muhleman, SMART Recovery Facilitator

Members of the LGBTQ+ community come to recovery with a unique set of issues. Please understand that these issues are not necessarily exclusive to the LGBTQ+ community, as anyone in a marginalized minority (defined by ethnicity, socioeconomic status, disability, etc.) would find commonality with the many issues that could be discussed. For the sake of this post, though, the discussion is from the LGBTQ+ perspective.
I recently read that compared to the general population, people identifying as LGBTQ+ are three times more likely to have a struggle with addiction (9% vs 30%)! This dovetails with a much higher incidence of co-occurring disorders, such as depression. Low self-esteem, anxiety, suicidal thoughts, and self-harm factor into this equation. Transgender persons tend to struggle with eating disorders at a far higher rate than the heterosexual population.
From where does this all come?
Though great strides have been made in the community, with gay/straight alliances on high school campuses and acceptance of same-sex marriage by the majority of Americans, vocal opposition to same-sex attraction and gender dysphoria has become more strident in the current political climate. Regardless in which era one has grown up since the Stonewall riots of 1969, anyone not fitting the heteronormative stereotype has experienced negative pushback from family, peers, or society generally. (It has been suggested that up to 40% of young male runaways do so over family rejection of the young man’s sexual orientation!)
The awareness that one is somehow “different” from the population at large coupled with negative familial or social messaging is not without its toll on a young psyche.
The toll this can take ranges from conscious thought in the form of toxic shame (“Something is wrong with me, I’m not normal, I am an aberration, a mistake.”) to subconscious, internalized homophobia, an unfortunate dislike of oneself due to sexual orientation or gender identity because the message is that a person in this category is not to be accepted or deserving of approval.
It is no wonder then that depression, anxiety, and other emotional disorders result. To find positive self-esteem in this light requires more than self-affirmations. Humans are familial and social. As much as we’d like our feelings of self-worth, that we’re okay, should not be dependent on influences from outside of us, what does one do when the negative message is ingrained in our thoughts or subconscious mind?
It is no mystery that substance use can provide an immediate, though temporary, respite from all this. A substance numbing negative feelings, allowing a person to feel okay being themselves can prove irresistible. No one partakes with the intention to become addicted, but the intensity of the need leads down that rabbit hole.
I will be the first person to say that the SMART Recovery process (the tools) is sexual orientation and gender identity agnostic. The process that puts an end to addiction is the same for everyone. However, the reason SMART offers meetings for the LGBTQ+ community (and other groups) is to provide a forum where common experience and unique understanding inform the conversation.
Though SMART tools are no replacement for therapies that can assist the conscious or unconscious change of mindset, they can elicit a self-awareness, a mindfulness, that can create a foundation to help such therapy be more effective.
Understanding the underlying factors leading to substance abuse enables one to better manage thoughts, feelings, and behaviors to end addiction.
By no means am I saying this applies to everyone in the LGBTQ+ community with a substance use disorder, but if estimates of co-occurring disorders are anywhere near accurate, they bear at least consideration as potential contributing factors to addiction. Dealing with toxic shame or internalized self-loathing concurrently with the SMART Recovery process should increase the chances of success many times over.
Watch Jeffry in his Facilitator Spotlight video.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

Alicia Renegar is a Certified Addiction Peer Recovery Coach and SMART Facilitator in Columbus, Indiana. As a gay woman, she faced much adversity and discrimination throughout her life. She shares how she has turned this negativity into strength and is helping others on their path to recovery.
In this podcast, she talks about:
- The challenges and discrimination she faced from administrators and peers during her school years
- How people’s fear of change impacts their decisions and attitudes towards what they perceive as different
- Her parents being very supportive and giving her a solid foundation to be who she is
- The journey to becoming herself
- How her deep-seated trauma pushed through and ultimately led to her addiction
- Volunteering then working for ASAP Hub
- Finding SMART and taking the facilitator training course
- Starting an LGBTQIA+ meeting in Columbus, Indiana
- Why SMART resonates with people
- The proudest moment of her life was becoming a Certified Addiction Peer Recovery Coach
- The obstacles and dangers of being an LGBTQIA+ activist
Additional resources:
Click here to find all of SMART Recovery’s podcasts
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

Persons like me in long term recovery can face horrible treatment if it becomes known we have had a substance use disorder. This is particularly true when we may need controlled substances as part of our legitimate medical care. There are now algorithms being used to scan our personal and medical data to see if we may be drug seekers. If you get identified as a drug addict, you are likely to get treated poorly, kicked out, and not helped. If we want to get more Americans into sustained recovery, we need to start treating people more fairly in our medical care systems. This must include fixing how we identify and provide care to persons with suspected addiction in our hospitals and doctors’ offices.
A number of years back, I had a dental emergency. I have had a few of those in my life, unfortunately. I had a procedure and the antibiotics the dentist gave me were not strong enough. The infection came roaring back with a vengeance. The side of my face looked like I had a golf ball in my cheek. It is the most pain I have ever experienced. A 10 on the pain scale. This occurred while I was visiting family in Western Pennsylvania. It got really bad in the middle of the night. I went into a rural hospital and asked for help. The staff took turns coming into the room to look at me. I was a sight, and I am sure everyone wanted to see the patient who looked like a squirrel with an acorn in his mouth.
They wrote out scripts for a more powerful antibiotic and gave me a strong opioid to provide some relief. I recall them mentioning it was addictive and if I knew that there were risks. I told them I was a clinician who worked in addictions, and I did know that the meds I needed that night were addictive. I did not tell them I was in recovery. I was afraid that they would leave me in excruciating pain. I have experienced horrible treatment at the hands of medical staff who became aware I had a history of substance use issues. It does not even matter that I am in recovery. I have had hundreds of patients I have worked with who recounted similar tales of unprofessional care at the hands of doctors and nurses. I could not tell them I was in recovery; I did not want the same to happen to me on this night with that agonizing pain.
I got the meds and went to stay with my family. I took the meds and switched over to an NSAID as soon as the antibiotics began to work. I let my family know I was taking an opioid. That is my standard protocol for the handful of times in 36 years of recovery I have needed to take medicine with an addictive potential. It was what I needed. I got through it fine with zero impact on my recovery. Society has a stigmatized view of people like me, that any use of a medication results in a relapse. It is simply not reality. It just means we need to be a little more cautious and practice good self-care. We are just as capable of doing so as a diabetic is capable of navigating a day with dietary risks.
I have been thinking after reading this journal article from the annals of Emergency Medicine, In a World of Stigma and Bias, Can a Computer Algorithm Really Predict Overdose Risk? Bamboo Health has developed software that gathers peoples data to determine an overdose risk score called NarxCare. It uses an algorithm and there are reports emerging that far too often patients with legitimate medical problems end up being scored as potential drug addicts. They are then treated like pariahs by medical professionals, not offered help but kicked to the curb and treated like criminals.
As this article notes, NarxCare gathers information like criminal records, sexual abuse history, distance traveled to fill a prescriptions and even pet prescriptions to assign risk scores to each person. Minorities score higher as our criminal justice system has historically targeted Black, Indigenous, and people of color for drug crimes and arrested them at higher rates than whites. Women who have more documented sexual trauma than men get scored higher. How does addiction treatment or self-identified recovery score on the algorithm? That is proprietary.
A recent and quite comprehensive legal review, published in the California Law Review, Dosing Discrimination: Regulating PDMP Risk Scores, by Jennifer D. Oliva, Esq, Associate Dean for Faculty Research and Development, Professor of Law, and Director, Center for Health & Pharmaceutical Law, Seton Hall University School of Law notes that:
“NarxCare risk scoring likely exacerbates existing disparities in chronic pain treatment for Black patients, women, individuals who are socioeconomically marginalized, rural individuals, and patients with complex, co-morbid disabilities and OUD.”
Professor Oliva has found that the software flags people who are rural and travel far for medical care or pay cash and use multiple payment methods. Such payment methods are often used by people who uninsured or underinsured. They scramble to try and find ways to pay for their medication.
If your sexual trauma history gets in your medical record, you may end up not being able to obtain the same medical care as others as you could get flagged as a potential drug addict at risk for overdose. As I noted, the software is proprietary. Not open for validation and not regulated. Oliva notes in her detailed legal review of the software that:
“there are no other examples of automated predictive risk scoring models created primarily for law enforcement surveillance that are used in clinical practice. This is likely because such cross-over use of risk assessment tools is ill advised. That stated, to the extent that clinicians do use PDMP risk scores to inform or determine patient treatment, PDMP software platforms ought to be subject to the same regulatory oversight as other health care predictive analytic tools used for similar purposes. The significant questions raised about PDMP risk score accuracy and such risk scores’ potential to disparately impact the health and well-being of marginalized patients demand immediate regulatory attention.”
This article at Wired.com writes about a woman who was kicked out of receiving services from her primary care provider. Her dogs were prescribed opioids and benzodiazepines. That gave her a high score for potential addiction. She became a person to be gotten rid of, not helped. She became a medial care pariah. She got the drug addict treatment, she was shown the door and terminated from care. This proprietary software influences medical care for millions of Americans. I found that Rite Aid uses it in Pennsylvania and 11 other states as does Walmart and CVS.
As noted above, it appears that instead of being used to help get persons who are at risk for addiction help, the software is often used to remove persons from care. I ran across countless stories where that was the outcome. This may stem from fear that doctors and pharmacist have of DEA sanctions. As persons on such medications face withdrawal as they are sent to the streets, it may actually result in increasing the overdose risks of patients it identifies as being at high risk.
When it is in error, there is little recourse for the patient. It is highly unlikely it will be corrected. Once you get flagged by this unvalidated proprietary software as a drug addict, good luck clearing it from your electronic health record. Persons in recovery have every reason to fear how the flow of such information will influence their treatment. We have a system of care designed to find and fail us. You have the right to request that something be removed from your electronic health record. Your medical provider is required to respond, but they can just say no. This study, done in 2014, found that if you requested a change to your medical record in regard to drug seeking behavior, your request had less than a 10% chance of being approved. Marked for life. The letter A for drug addict written into your EHR for eternity.
As addiction is a medical disorder, we should be providing medical care to a person with a substance use disorder as we would say a diabetic. Without judgement and with the same care and concern as any other patient. We do not do so in America. Being treated like a drug addict in America means being treated like an outcast. A member of an unclean caste. This says a lot about how far we have to go in respect to proper care for addiction in America.
What other medical condition would the use of unvalidated, proprietary software be used to guide medical care? Hundreds of thousands of persons like me across America are forced to think about medical care bias against us every time we seek help. We must change how we treat people with substance misuse issues and those of us in recovery. We need to be cared for respectfully and with compassion, just like what we expect for any other medical condition.
Last year, I wrote this piece, “Take the Drug Addicts Out to the Hospital Parking Lot and Shoot Them.” I suggested then we need stronger privacy laws and that we must hold medical professionals accountable for discrimination in the treatment of persons having or suspected as having a substance use disorder. We need to have zero-tolerance policies on discriminatory treatment of persons with a substance use disorder written into every hospital policy. They should include strong administrative sanctions for all staff who discriminate against us and everyone who witnesses it and fails to report it. Put such policies in place in every medical institution in the country.
How can we get more people into recovery in a system of care that acts so punitively towards us? If we want to increase the number of Americans in recovery, we must improve the care provided to persons with substance use disorders. We need to ask hard questions about how such algorithms impact a person who has or is suspected of having a substance use disorder. We must receive the same standard of care as everyone else. We must stop medical care bias against us.
We will know when we have a healthcare system that works for persons like me with substance use disorders when people like me do not have to be afraid of being identified as having a history of substance use disorders in our medical care systems. When we experience no shame, no negative judgment, and no disparate care we will have arrived at where we need to be. A day when we no longer live in fear of these algorithms of discrimination. We have a long way to go to meet that standard, but we must work towards it if we are to actually help the millions of Americans who need help with a substance use disorder.
