
Just because Tim Burton had a previous career in the steel industry doesn’t mean he’s hard-headed. In fact, Tim is open-minded and willing to learn, which has led him to where he is today: a Volunteer Support Specialist (VSS) for SMART.
He felt a calling to work in the addiction and recovery field after working in a hospital, and it became a pursuit a couple of years ago. “I found a job with a Recovery organization working in KY counties where [Opioid] overdose rates were the highest. From there I discovered SMART and became a facilitator.”
As a VSS, Tim loves hearing from volunteers who are excited to be starting out as meeting facilitators as well as seasoned facilitators sharing their passion for SMART. He helps all those who need it.
Here are Tim’s responses to the Take 5 Spotlight questions:
- Are there tasks you perform regularly during your workday? Right now, it’s all about the audit we are doing to clarify meeting status across the US, but in my spare time it’s about learning all the other job functions—there is a lot to learn.
- What are a couple of the ways you interact and coordinate your job with other national office staff? The Volunteer Department touches everything else in SMART Recovery, it’s really the backbone of the whole organization.
- What is one of the ways that you think you personally make a difference at SMART? My background is so diverse that I hope to be a utility player that makes a difference. Put me in coach, I’m ready to play!
- What is your message to all those dedicated SMART volunteers across the country? Discouragement is your enemy and don’t try and shoulder it alone. Call me!
- What kinds of things are you interested in outside of work? Any hobbies? Just about any human power sport. I’ve backpacked over 200 miles of the Appalachian Trail since 2020, my wife and I love kayaking, and cycling is my lifelong passion. Sunday morning finds me in church somewhere.
Whether you find Tim on the trail, in the water, on wheels, or sitting reflectively, you’re sure to understand one thing: he loves SMART and helping people. A powerful combination and a great contribution to SMART’s Volunteer Support Department.
Learn more about the Take 5 Spotlight series and see others who have been profiled.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

For Alena Kuplinski, a SMART employee who splits her work responsibilities between the Call Center and Volunteer Headquarters (VHQ), her success at SMART came by way of Poland. As in the country of.
Alena lived in Poland for five years and says it set her up for success in dealing with all kinds of people, “I was lucky enough to meet and work with people from all around the world, [I learned] to communicate effectively across language barriers and cultural differences.” This meant she became a great listener & communicator, and that’s essential for the work she does.
Her VHQ activities include keeping track of new meetings, making necessary changes to existing ones, registering volunteers, and anything else that needs done. In the Call Center she handles the broad array of inquiries that flood the SMART phones.
One specific connection she has to SMART is through her father, who has been a participant in meetings trained facilitator, and is now Regional Coordinator for Nevada. This provided a close-up view of SMART’s value, “Seeing how much SMART helped him really made me have a lot of passion for the organization as I have witnessed firsthand just how much it can change lives.”
Here are Alena’s responses to the Take 5 Spotlight questions:
- Are there tasks you perform regularly during your workday? The first and foremost task is taking care of meeting changes to make sure our list is up to date and accurate, so that those wishing to attend a meeting are getting the correct information. Another task I do regularly is answering our Contact Us emails in our VolunteerHQ inbox. And of course, answering phones!
- What are a couple of the ways you interact and coordinate your job with other national office staff? Those of us in the National Office make effective communication a top priority. We keep in touch via Zoom both through messages and calls, as well as emails, to make sure that we are helping everyone that needs help.
- What is one of the ways that you think you personally make a difference at SMART? Between my work in the Call Center and VolunteerHQ I spend a lot of time interacting with the participants of our meetings as well as our facilitators. I feel like this gives me a special opportunity to help people in all aspects of their recovery and involvement with SMART.
- What is your message to all those dedicated SMART volunteers across the country? I am endlessly impressed by the dedication of our volunteers and without them SMART would not be what it is. Thank you for all of your hard work!
- What kinds of things are you interested in outside of work? Any hobbies? I’m a huge music lover and spend a lot of time listening to music, attending concerts, and practicing bass. I also enjoy reading, writing, playing video games, traveling, and cooking.

The music that SMART Recovery hears when it comes to Alena Kuplinski is a fluid melody of listening, responding, and helping. That’s the kind of song that makes SMART function like a well-tuned orchestra.
Learn more about the Take 5 Spotlight series and see others who have been profiled.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

The DrugWise Daily newsletter noted the passing of Sara McGrail.
I never met Ms. McGrail and I didn’t follow her work, but her name rang a bell. I knew I’d interacted with her years ago but couldn’t remember the details.
It turns out we interacted around some posts related to harm reduction in 2008.
I had posted a response to something she wrote, she respectfully and thoughtfully responded. A couple of months later, we had a similar exchange that resulted in my conceptualization of recovery-oriented harm reduction.
This was an outcome of her meaningful engagement in the face of our disagreements, and her challenging, vigorous, substantive, and good faith arguments.
We saw things differently, but her questions, assertions of her values, and her prodding challenged me to examine my convictions and made me more thoughtful.
As I said, my knowledge of her and interaction with her was limited, and I don’t know if it was typical of her. Whatever the case, I am grateful to her for challenging me to think more deeply about the intersection of harm reduction and recovery.
What is recovery-oriented harm reduction?
Recovery-oriented harm reduction (ROHR) seeks to address the historical failings of both abstinence-oriented treatment and harm reduction services. ROHR views recovery as the ideal outcome for any person with addiction and uses recovery (for addicts only) as an organizing and unifying construct for treatment and harm reduction services. Admittedly, these judgments of the historic failings are my own and represent the perspective of a Midwestern U.S. recovery-oriented treatment provider.
Addiction is an illness. The defining characteristic of the disease of addiction is diminished and/or loss of control related to their substance use.
Drug use in addiction is not freely chosen. Because the disease of addiction affects the ability to choose, drug use by people with addiction should not be viewed as a lifestyle choice or manifestation of free will to be protected. It is not an expression of personal liberty, it is a symptom of an illness and indicates compromised personal agency.
All drug use is not addiction. There is a broad spectrum of alcohol and other drug use. Addiction is at the extreme of the problematic end of that spectrum. We should not presume that the principles that apply to the problem of addiction are applicable to other AOD use.
ROHR is committed to improving the well-being of all people with addiction. ROHR services are not contingent on recovery status, current AOD use, motivation, or goals. Further, their dignity, respect, and concern for their rights are important are not contingent on any of these factors.
An emphasis on client choice—no coercion. While addiction indicates an impaired ability to make choices about AOD use, service providers should not engage in coercive tactics to engage clients in services. Service engagement should be voluntary. Where other systems (legal, professional, child protection, etc.) use coercive pressure, service providers should be cautious that they do not participate in the disenfranchisement or stigmatization of people with addiction.
For those with addiction, full recovery is the ideal outcome. People with addiction, the systems that work with them, and the people around them often begin to lower expectations for recovery. In some cases, this arises in the context of inadequate resources. In others, it stems from working in systems that never offer an opportunity to witness recovery. Whatever the reason, maintaining a vision of full recovery as the ideal outcome is critical. Just as we would for any other treatable chronic illness.
The concept of recovery can be inclusive — it can include partial, serial, etc. While this series argues for a distinction between recovery and harm reduction, Bill White has described paths that can be considered precursors (precovery) to full recovery.
Recovery is possible for any person with addiction. ROHR refuses cultural, institutional, or professional pressures to treat any sub-population as incapable of recovery. ROHR recognizes the humbling experiential wisdom that many recovering people once had an abysmal clinical prognosis.
All services should communicate hope for recovery. ROHR recognizes that hope-based interventions are essential for enhancing motivation to recover and for developing community-based recovery capital. Practitioners can maintain a nonjudgmental and warm approach with active AOD use while also conveying hope for recovery. All ROHR services should inventory the signals they send to individuals and the community. As Scott Kellogg says, “at some point, you need to help build a life after you’ve saved one.”
Incremental and radical change should be supported and affirmed. As the concepts of gradualism and precovery indicate, recovery often begins with small incremental steps. These steps should not be dismissed or judged as inadequate. They should be supported and possibly even celebrated and they should never be treated as an endpoint. Likewise, radical change should not be dismissed as unrealistic or unsustainable pathology.
ROHR looks beyond the individual and public health when attempting to reduce harm. ROHR wrestles with whether public health is being protected at the expense of people with addiction, whether harm is being sustained to families and communities, and whether an intervention has implications for recovery landscapes.
ROHR should aggressively address counter-transference. ROHR recognizes a history of providers imposing their own recovery path on clients while others enjoy vicarious nonconformity or transgression through clients. These tendencies should be openly discussed and addressed during training and ongoing supervision.
ROHR refuses to be a counterforce to recovery. ROHR seeks to be a bridge to recovery and lower thresholds to recovery rather than position itself as a counterforce to recovery. Recognizing that addiction/recovery has become a front in culture wars, ROHR seeks to address barriers while also being sensitive to the barriers that can be created in this context. When ROHR seeks to question the status quo, it is especially wary of attempts to differentiate from recovery that deploy strawmen, recognizing that this rhetoric is harmful to recovering communities and, therefore, to their clients’ chances of achieving stable recovery.
ROHR sees harm reduction as a means to an end. ROHR views harm reduction as strategies, interventions, and ideas to reduce harm. As such, it is wary of harm reduction as a philosophy or ideology, which sets the stage for seeing harm reduction as an end unto itself. Back to Scott Kellogg’s point, “at some point, you need to help build a life after you’ve saved one.” The end we seek is recovery, or restoration, or flourishing. Seeing harm reduction as a philosophy or ideology risks viewing it as “the thing” rather than “the thing that gets us to the thing.”
 Codependent is a word that is thrown around rather loosely, but what does it really mean to be codependent? By definition a codependent person is one who has let another person’s behavior affect him or her and who is obsessed with controlling that person’s behavior. As you might imagine most people are not fond of this definition and do not want to see themselves as either controlling or obsessed. It can be helpful to substitute the words concerned for obsessed and helping for controlling, as those words tend to be more palatable to most.
Codependent is a word that is thrown around rather loosely, but what does it really mean to be codependent? By definition a codependent person is one who has let another person’s behavior affect him or her and who is obsessed with controlling that person’s behavior. As you might imagine most people are not fond of this definition and do not want to see themselves as either controlling or obsessed. It can be helpful to substitute the words concerned for obsessed and helping for controlling, as those words tend to be more palatable to most.
The reality is the only way someone suffering from substance use disorder can continue their addiction is if someone else is cleaning up the wreckage of it. In its truest form codependency is obsessive ‘helping”, doing things for another adult that they can and should be doing for themselves.
While it is healthy to feel concern for someone we love, codependency uses this concern to justify boundary violations as attempts to “help” the person we love. The only way we feel better is to make the substance user feel better by trying to fix their problems. We pay their bills, take care of their legal issues, cancel our plans in order to meet their needs, lie for them, and the list goes on. As long as we continue to rescue the substance user from the consequences of drinking and using, that person will use. It’s as simple as that.
Signs of codependency include:
- Offering advice to others whether it is asked for or not.
- Taking everything personally
- Lying or making excuses for another person’s behavior
- Using manipulation, shame, or guilt to control another person’s behavior
- Feeling responsible for other people’s problems
- Expecting other’s to respond a certain way
- Feeling like a victim
- Fearing rejection
- Feeling used and underappreciated
- Confusing being loved with being needed
In our society, codependency can be as deceptive as addiction. It hides behind the guise of helpfulness, “doing the right thing”, taking one for the team, or being a loving parent/spouse/child/partner/friend. It is a way of avoiding our true feelings by instead focusing on managing our external world. Codependent people often lose sight of where they end and other people begin. The boundaries are blurred or nonexistent.
If you are in a relationship with someone struggling with a substance use disorder, it is natural to experience a desire to help. It is tempting to believe your efforts to help your loved one will stop them from using. This is simply not true. The truth is focusing on your own recovery, finding peace and healing for yourself is the greatest gift you can give the people in your life. You’re worth it!
Written by:
Kelly S. Scaggs, LCSW, LCAS, CCS, MAC, ICAADC
CLINICAL DIRECTOR, Fellowship Hall
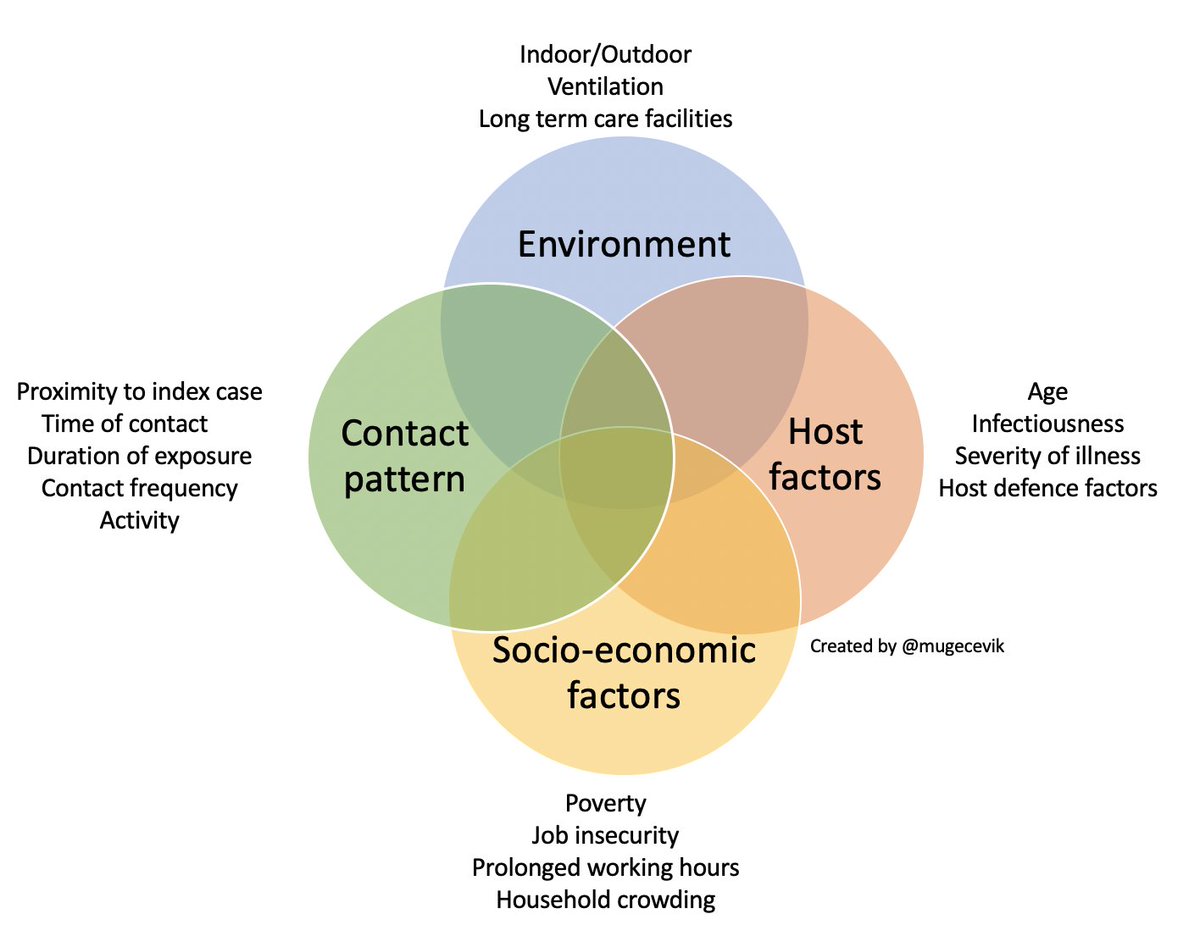
Tweeted by Muge Cevik on September 21, 2020
One argument against the disease model of addiction is that it advances a narrow medical model at the expense of recognizing social and environmental epidemiological considerations, as well as social and environmental interventions.
This image does a good job demonstrating that calling something a disease often should not necessitate a narrow medical approach. The graphic below focuses only on factors influencing transmission. Obviously, environmental and socio-economic factors don’t cause COVID, but they do influence risk, and that reality doesn’t make COVID any less of a disease.
I imagine a similar graphic could be made to represent the treatment and management of COVID that would include medical treatments as well as other factors and strategies (environmental, social, psychological, spiritual, etc) that influence access, engagement, compliance, response to treatment, and the pace stability of the patient’s recovery.
The import of those “nonmedical” dimensions only grows when we’re looking at chronic diseases that require management because there are no cures.
If AOD problems could be solved by physically unraveling the person-drug relationship, only physicians and nurses trained in the mechanics of detoxification would be needed to address these problems. If AOD problems were simply a symptom of untreated psychiatric illness, more psychiatrists, not addiction counselors would be needed. If these problems were only a reflection of grief, trauma, family disturbance, economic distress, or cultural oppression, we would need psychologists, social workers, vocational counselors, and social activists rather than addiction counselors. Historically, other professions conveyed to the addict that other problems were the source of addiction and their resolution was the pathway to recovery. Addiction counseling was built on the failure of this premise. The addiction counselor offered a distinctly different view: “All that you have been and will be flows from the problem of addiction and how you respond or fail to respond to it.”
Addiction counseling as a profession rests on the proposition that AOD problems reach a point of self-contained independence from their initiating roots and that direct knowledge of addiction, its specialized treatment and the processes of long-term recovery provide the most viable instrument for healing and wholeness. If these core understandings are ever lost, the essence of addiction counseling will have died even if the title and its institutional trappings survive. We must be cautious in our emulation of other helping professions. We must not forget that the failure of these professions to adequately understand and treat addiction constituted the germinating soil of addiction counseling as a specialized profession.
White, W. (2004). The historical essence of addiction counseling. Counselor, 5(3), 43-48.
It’s important to note that William White specifically refers to addiction counseling. (If he were writing this today, I imagine he might consider replacing “AOD problems” with “addiction” or “severe AOD problems.”)
I’m often asked why I believe it’s so important to understand addiction as a primary illness. It’s because professional helpers need to know that attempts to resolve addiction by addressing other problems are generally doomed to fail. We can house people with addiction, treat their trauma, treat their mental illness, give them supportive employment, legalize drugs, provide drug testing supplies, clean works, regulated supply, and guaranteed minimum income. Even with all of that support, they are still likely to die of untreated addiction.
Even when we effectively treat opioid use disorder, cocaine use disorder, or alcohol use disorder, we may still be setting the stage for them to suffer or die of untreated addiction. For example, a patient’s opioid use disorder may be effectively treated and the patient dies of causes related to their alcohol or stimulant use. Or, their impairment and it’s consequences persist due to misuse of co-prescribed benzos and stimulants.
This was Narcotics Anonymous’s breakthrough idea in the 1950s–that the problem should not be conceptualized as alcohol or heroin or cocaine, but addiction.
NA’s definition of the problem as a process of “addiction” that transcended one’s drug choice and required a common recovery process may be viewed by future historians as one of the great conceptual breakthroughs in the understanding and management of severe alcohol and other drug problems. This is all the more remarkable coming at a time that substance-specific disorders were still thought to be distinct from each other, as were their treatment and recovery processes.
Budnick C, Pickard B & White W. (2011). Narcotics Anonymous: Its History and Culture
To say that addiction is a primary disease and not caused by these other problems does not imply that these problems are unimportant, or that they have no relationship to addiction. These other problems may be secondary to addiction, or they may also be a co-occurring primary problem.
In either case, these problems may affect the risk for addiction, the onset, its course, severity, and response to treatment. They may represent a barrier to recovery. And, importantly, they cause suffering.
This is why addiction counseling as a specialty is so critically important. In most cases, recovery from addiction is not catalyzed by character development, mental health treatment, housing, or trauma treatment.

We saw a huge surge in alcohol misuse from the very earliest days of the COVID 19 pandemic. Americas most socially acceptable drug of misuse helped sooth a lot of rattled nerves. But, if one argument for normalizing drugs use stems from the belief that doing so will decease problematic use, we may not want to use alcohol as our poster child for success. Even before the pandemic, this National Institute on Alcohol Abuse and Alcoholism (NIAAA) article noted that between 1999 and 2017, we lost nearly one Million Americans to alcohol related deaths. One million human beings. It is a big number, but we tend to ignore these deaths as a nation. Alcohol misuse is stealing lives, right under our noses. Have we normalized these losses in ways we should not have? What, if anything are we going to stop these deaths?
Some of the early (and grim) stats on the pandemic and alcohol related deaths are starting to come in. A JAMA study found a 25.5% increase in alcohol related mortality during the pandemic. These deaths were steadily increasing prior to the pandemic. As it states, “drinking has been going up for 10 or 15 years among adults, and the trend accelerated in 2020, as some of the motivations to drink changed: Stress-related drinking increased and drinking due to boredom increased.” One researcher is quoted as hoping it may go down, but also acknowledges that this may be our “new normal.” Even as these deaths are burgeoning, we ignore them. We normalize these devastating losses. Why?
Alcohol has probably been one of the primary ways that people have numbed themselves through the trials and tribulations of the pandemic. This NBC article talks about the rise of “mommy juice” memes of women mixing Whiskey with their Sprite to get through the day and navigate multiple roles of childcare, work and every other responsibility. It is way more convenient to get wasted on alcohol than ever. Here in Pennsylvania, if you want some alcohol infused gelatin shots for the road, nearly every convenience store within ten miles of my home sells them now. These fruity concoctions and other similarly flavored alcohol related products that appeal to kids are everywhere. We should pay attention to the impact that they have on young developing brains wired for trying new things that Dr Judith Grisel talks about in her piece on the addiction trap. Early life use increase addiction over the lifecycle, but it is also market share for the companies that make these products. Perhaps that is one factor in why we are where we are at.
Like other medical conditions, recovery is easier earlier in the progression of the disease than in later stages. Yet, we largely ignore early cues associated with misuse when we see them. It is too uncomfortable for us to talk about, a direct impact of stigma. We generally allow the condition to worsen as it progresses while we work hard to look the other way. Yet, while alcohol use is acceptable, we don’t see alcoholism in the same light. When it gets to elephant sitting on the coffee table size of a problem, then we act. We act when people get arrested or are too impaired to hold down their jobs. We ignore what is visible in earlier stages until it is in its later, harder to treat phases. We do too little, too late.
We seem to now falsely view alcohol as less lethal for addicted persons than it truly is. This may be partially because we have had our eyes focused on the very real devastation stemming from the opioid epidemic, which also benefited big pharma companies so we looked the other way on that one for years, too. I hear of people getting life sustaining meds for an opioid disorder even as their severe alcohol use disorder is ignored. Preventing an overdose is laudable, but it is a waypoint, not an end goal, particularly for those of us experiencing other, largely unaddressed addictions.
We should consider what flourishing looks like for our patients and help them get there. Ask what you would want for your own mother or father, brother or sister, son or daughter, and that is what every person should get in respect to SUD care. We don’t deliver anything close to that. We should be doing some soul searching as to why we do not do so.
I have observed access to treatment barriers for alcohol use disorders because persons with Opioid Use Disorders (OUD) were prioritized for care. We ask about OUD at the door because there is funding to help persons with that disorder. Single diagnosis funding for an increasingly multi-use disorder! Can you imagine if we only treated one or two forms of co-occurring cancer? That would be morally wrong. If it is wrong for other conditions, why do we do it for addiction?
That programs end up having to triage care based on which substance they have funding is part of a larger problem. We are simultaneously plugging and drilling holes in the bottom of our proverbial boat. Addiction kills, recovery saves lives. Every addicted person deserves recovery, no matter which or how many substances they used. Every life, every time. Instead, we look the other way or ask why they chose to do this to themselves even as the science tells us it simply does not work this way. We do so because we still see addiction, including to alcohol as a moral failing. Sad but true.
I would be the first to admit in active addiction (including to alcohol) I posed a significant public safety risk. The unvarnished truth is that getting people like me into recovery can save a lot more lives than our own. There is a public safety imperative to support recovery. This week, here in Pennsylvania a young and intoxicated driver ran over and killed two state troopers and a citizen. We are rightfully flying state flags at half-mast for them. A tragic accident, but certainly not an isolated event. The 2020 National Highway Traffic Safety Administration report shows that alcohol impaired driving increased 29% over 2019, while alcohol related highway fatalities increased by 24%. This recent New York Times article notes the 25% jump in overall alcohol mortality and speculates that some of it may be related to increased resumption of use rates in recovering people. We had opportunities to more fully address these challenges and we did not do so. Why are we not doing more to get people into recovery simply as a matter of public safety?
When we do fund solutions, we ignore perhaps one of the most effective ones we have in front of us. We don’t fund recovery. We know that recovery is the solution, yet few resources get to the ground. Had we gotten resources to the recovery community pre-pandemic, I suspect it would have offered some protective benefits and helped reduce the SUD resumption rate. In hindsight, it would have been a penny on the dollars return on investment. Yet despite unprecedented funding from Congress to the states, many of our grassroots recovery community organizations still self-fund through bake sales and social media campaigns as we recently noted in a Stat News article coauthored with Ryan Hampton. Why? Recovery is in many cases the last in line for funding because we are still a stigmatized community.
What could we do to turn around the alarming increase in alcohol related mortality in America:
- Stop Looking the Other Way: Denial and avoidance does not work with addiction. It never has. We must face what is occurring and more fully address these issues in our communities. We must do so from a strength based, recovery orientation rather than the punitive focus we have for so long held in this country.
- Address the Subtle Dynamics of Stigma: To better address addiction, including to alcohol, we must normalize recovery. We have not learned how to talk about problematic alcohol use and to discuss it as a society. On some fundamental level see people who end up with a severe substance use disorder as having a character flaw or as morally compromised. We are still largely perceived as outcasts, an unclean caste. When people can live openly in recovery, it will be a lot easier to talk about addiction in a proactive way. Based on the national survey my organization did with RIWI and Elevyst, we have a long way to go until we reach that goal. There is no better time to focus on changing this sad fact than right now. We are not unclean; we are pillars of hope in our communities.
- Fund Recovery Community Organizations: Recovery Community Organizations (RCO) were conceptualized to wrap people in communities of healing. Recovery capital generators in our communities. Focused on getting us into and to sustain our recovery over the long term. Designed to support us getting back to work, taking care of our families and to be civically engaged contributors to our communities. The best possible outcome, people who are productive and contribute to our communities instead of destroying them. It is a common outcome. Let’s fund recovery to save lives!
- Focus on Early Interventions: Alcohol use disorders are killing us. We must address them earlier in the disease process while understanding that unaddressed addiction is public health and safety issues for our entire society.
- Increase Peer Mentoring Roles: We need to elevate lived experience within and across all of our social and governmental institutions. Visible examples of people in recovery serves up hope to those still struggling. It can open us up as a society to the difficult and life saving conversations we must have if we are to save more lives. We see effective models in our professionals in recovery organizations for lawyers and doctors. An early intervention may look a lot like a friendly conversation of concern from a colleague, opening the door to recovery. We should see these across all our employers and institutions, but we must form and fund them if we want this outcome.
Rarely in recent years have we even talked about the steadily increasing deaths from alcohol. Instead, we normalized them. Those losses were overshadowed by the opioid epidemic. One million dead from alcohol related mortality in the years immediately preceding the pandemic. Now it is 25% higher in the blink of an eye. Is it enough for us to pay attention to what is happening? We have improperly normalized the deaths of our fellow humans. We do so because we still do not see people who are addicted to even our most socially acceptable drug as people worthy of helping. If we did, we would have a fully funded system of SUD care that included RCOs and long term, recovery-oriented outcomes. We do not have that in America. We can have that if we decided to do so. When will we? What will it take to do so?
Problematic alcohol use is happening right under our nose, and the consequences are increasing even as solutions are under our noses. Yet even now, very little changes. How many more million loved ones must we lose before we focus resources on recovery using whatever pathways of recovery work for each person? The solutions may be difficult, but not nearly painful as normalizing the lost of hundreds of thousands more of our loved ones to alcohol use disorder.
The answer, which is investing in recovery. It is about time we do that.
Ted Perkins, aka the “Tips & Tools Guy” is a SMART facilitator and producer of our popular SMART Recovery video series including Tips & Tools for Recovery That Works, Life Beyond Addiction, Facilitator Spotlights, and more. A natural skeptic and avid humanist, he has always been open to ways to better himself, especially in his recovery. One way in which he’s done this is looking into the possible therapeutic value of psychedelic drugs. In this podcast he openly shares some of his experiences with people so they can understand the powerful impact they made in his life.
In this podcast, Ted talks about:
- How alcohol was normalized growing up in other countries
- His path from college to the entertainment industry being full of parties and substances
- Realizing he was living a suboptimal life because of alcohol
- Finding SMART and becoming a facilitator
- Trying LSD in the 1980’s and integrating the experience into his ongoing relationships
- Trying to be the best Ted he can be
- Learning about the popularity of psychedelics to aid in recovery
- His experience at a psychedelic summer camp in Costa Rica
- Being treated with Ketamine by his therapist
- The connection between his psychedelic experience and using SMART
- Getting what you need, not what you want
- Having a deeper emotional connection to the people in his life
Additional resources:
Click here to find all of SMART Recovery’s podcasts
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

Shardae Sharpe started college at 15 years old. Not having parental control and mental maturity, she began drinking alcohol. Her substance use continued all while she was struggling with school and relationship issues. Her path to recovery didn’t start with SMART, but through her job at Sober Grid, she has learned the program and is now taking the facilitator training course.
Subscribe to the SMART Recovery YouTube Channel
Video storytelling is a powerful tool in recovery, and we are proud to share our SMART Recovery content free-of-charge, available anywhere, on any device. Our videos hope to inform, entertain, and inspire anyone in the recovery community.
Subscribe to our YouTube channel and be notified every time we release a new video.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

Loretta Billingsley has been working in the media industry since the 1980’s and still loves what she does to this day. Another thing she loves is facilitating the SMART Women’s meeting on Saturday mornings. Loretta knows the personal growth and connections formed during those meetings have helped change lives, and for that she is grateful.
In this podcast, Loretta talks about:
- Being one of the pioneer women who started the women’s meeting
- Why the meeting has grown in popularity in the last year
- Notable guest speakers from the recovery community
- Her four levels of collective sharing
- Why inclusivity needed to be a part of the SMART community
- How we’re all recovering from something
- Humanity being the great connector
- Using practices instead of tools
- The journey down a new road of recovery
Additional resources:
Click here to find all of SMART Recovery’s podcasts
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
