Forward – I recently learned that Tom Hill was retiring from government work and concentrating on his art, another one of his many talents. My first reaction was a feeling of abandonment. We tend to see some people and the roles that they serve almost as permanent fixtures. Tom Hill has been that kind of fixture in the recovery community. If Bill White is our navigator, the Switzerland of neutrality and protector of our common ground, Tom Hill is our rudder. He has always had his pulse on the community. A lot of people, present company included, have depended on Tom for his wise counsel and a whole lot of insight on our shared values and what to do to stay on course and keep our ship afloat.
I am working on a side project to explore how people in recovery serving in government are able to navigate these difficult waters and do it in ways that remain true to themselves and our community. The idea for the project came out of a conversation I had a few months ago with Bill White. Getting this interview was vital for what I want to accomplish. Tom was kind enough to set down his palette and brush and talk with me for an hour.
It now occurs to me that there is more than one way to lead. Tom is stepping away from his formal recovery community role to be true to himself. Showing us the way forward, practicing self-care and following his path of growth. As this interview reflects, one of the lessons in recovery is to keep your feet on the ground and to take that next step. Tom is practicing what he preaches. As the feeling of abandonment faded, it was replaced with deep respect and a sense of awe for how recovery unfolds in our lives and the power of letting ourselves flow in that current. Thank you, Tom!
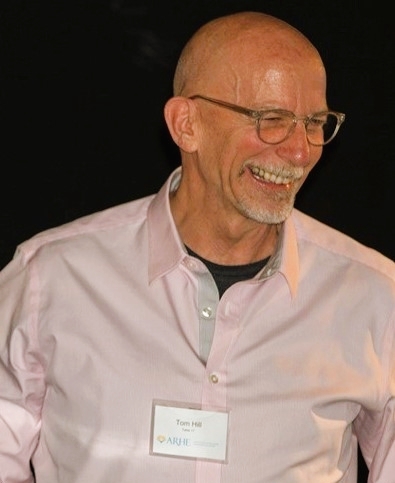
Tom Hill retried last month from his position as senior policy advisor at the White House Office of National Drug Control Policy (ONDCP). Prior to that position, he served as the Vice President of Practice Improvement for the National Council and a Presidential Appointee in the position of Senior Advisor on Addiction and Recovery to the SAMHSA Administrator. At one point, he served as Acting Director of the Center for Substance Abuse Treatment. He also helped PRO-A, our statewide RCO here in Pennsylvania to adopt our current organizational framework. Tom has also used his role in the policy realm to develop recovery-oriented systems of care and support efforts to get more people into long term recovery. He is humble and hardworking. Tom is the recipient of numerous awards, including the Johnson Institute America Honors Recovery Award, the NALGAP Advocacy Award and a Robert Wood Johnson Fellowship in the Developing Leadership in Reducing Substance Abuse initiative.
I only ask of Tom that he lets us know of his next galley opening. I want to see what he is putting on his canvas in this new chapter. I know I am not the only one who wants to celebrate what comes next!
- Thinking back to your early days of recovery, what or whom influenced the values around recovery that shaped who you were and what you have accomplished?
I want to start by noting that my career was not a planned path, it was the one that was revealed to me over time. When I think back to those early days of recovery, it is important to note that everything about recovery went against all I had learned about how to get ahead in the world. I grew up in DC. I was taught to be tough, to always be in control, not to ask for help and that to be kind was to be weak. A lot of the business world and even government runs this way as well. Recovery introduced me to an alien world that ran counter to how I lived up to that point. This new way changed my life. This new way saved my life.
One of the important things to understand is that I never set down a plan to have a career centered on recovery or to work inside government. What happened for me was more of an organic process. I worked on the issues that had meaning to me and the rest simply unfolded. The values I learned in early recovery were foundational in both my personal life and my professional work. The values of recovery were things I had to slowly open up to. They really changed my whole world. To be able to let go of control and trust the process. To strive to be honest, to live with integrity, to have a purpose greater than oneself. The foundation of love and kindness…were not who I was before I got into recovery. I had lived contrary to these values.
I had a good sponsor, and I was in therapy. I did not have any idea of what trauma was. I remember hearing about Adverse Childhood Experiences (ACEs) and realizing I had a high score. I learned what all that was about. It made a lot of what happened in my life and how I responded to things make sense. Understanding “the why” helped, as I have matured, the why is less important now, but at the time it really helped me understand a whole lot. I began to heal.
In reflection, I think my recovery foundation really did shape me. When I think of these values, the very values that shaped so many of us, they are seen as pretty radical out in the rest of the world. Most institutions do not work under such values. We can end up in conflict fairly easily with systems that do not operate in the way we learn to do to sustain our recovery. It can be a real struggle to stay true to these values out in the world.
- You were part of the first cohort of the Recovery Community Support Project (RCSP) through SAMSHA, the first time that recovery community organizations were funded in America. What influence did that process have on you and the work you have been involved with over the last two decades?
I think back to those early RCSP days, and it was really a miracle that this group of people came together. There were so many amazing people in the first and second cohort. It was really incredible when you think about it. SAMHSA Grant officer Cathy Nugent and June Gertig, Project Director for the RCSP Technical Assistance Project helped focus us in ways that focused our work. One of the most remarkable things was that they had a deep understanding of the power of community. Valuing community is fundamental to developing effective strategies, but often times our institutions approach things from a top-down approach, not including communities in solutions at all, or only in pro forma way.
Community needs to be central player in change strategies, but it often ends up as window dressing as other “legitimate” institutional goals are pursued. If you really want to help a community, you provide it with the resources and support it needs to solve its own problems. That is what works and what government repeatedly fails at. Agendas are rolled out and conducted in ways that far too often fail to harness the power of community by engaging it in its own healing process. Top-down approaches tokenize the recovery community, with the message that people, families, and communities are not capable of finding their own solutions. Communities from all around have proved this wrong. The recovery community has proved it wrong in capital letters.
The Recovery Community Support Program is an excellent example of one of those rare instances in which government valued “community up” solutions. What a miracle was that – the right people were in the room. The cohort included people like Don Coyhis, Phil Valentine, Joe Powell, Bev Haberle and Dona Dmitrovic. You had grant officers who understood how community up problem-solving works and you had this amazing group of people assembled from across the country who all came together. This SAMSHA project that was really run on a shoestring budget, it sort of bumped along. But it had its champions, like Dr H. Westley Clark CSAT Director and Rick Sampson, the Director of the Division where the RCSP was housed. Without their support it would not have achieved what it did.
The back story was that when the project was conceived, there was a sense that SAMHSA would facilitate this project, people and organizations would be developed and the focus would be to remove barriers to treatment. This was in the era when recovery month was focused on Treatment Works! as a slogan. The thing was, when all these people came together, it was realized that this is not what our communities wanted to do. There were such varied pathways to recovery, many included treatment, many did not. The cohort wanted to focus on strengthening recovery. The miracle was that, by listening to the reports from community leaders, the government started trusting and valuing the lived experience and wisdom of the recovery community. At the end of the day, that is the miracle that gave the recovery community a foothold in government.
- You have had quite an impressive career in government. You were one of the highest government officials openly in recovery. How have you navigated the values of recovery representation in these positions?
As we have talked about, I never had a master plan to do this. I honestly think I was called to this work, as I think you and many of us have been. Occasionally, messengers show up and give us a nudge. The truth is that when I was initially asked a few of years back if I wanted to pursue an available position within government, I said no. I couldn’t really picture myself in that role. Working for a government contractor doing technical assistance, I felt that I had more freedom working directly with the recovery community.
After I said no, the agency official came to me again and asked if I would consider a time-limited role, as a political appointee. I certainly saw that there was potential for me to further some of objectives of the recovery movement, alongside my friend and colleague, Tom Coderre, who was already serving. I got on the phone and ran the idea by many of my colleagues and decided that I could not afford to turn down the offer. The idea was very compelling, I ended up saying yes, not once but twice. So, I ended up in government.
Earlier I spoke about how the priorities of government and the values of recovery can come in conflict. It can make the work difficult, and I believe that it is beyond helpful to have a program of recovery to navigate these conflicts. Without that, I know I would lose their way quickly. Government works at its own speed. You often do not know how well you are carrying the water because everything is so heavily steeped in politics and frequent changes are constant. “Keeping it simple” can seem impossible in an arena of complicated decision-making and a variety of changing factors. Because government moves very slowly, working to make sustainable policy and systems change takes both short-term and long-term strategies, along with a whole lot of patience and stamina. Seeing a project gain momentum and then sputter can be disheartening, requiring us to keep our determination fixed on the end goal, which may take substantial time to realize.
For me, it has been important to stay rooted in recovery values in all the places I have worked and especially in government. At the end of the workday, I have to ask myself questions like: was I honest, was I fair, did I listen well, did I do what I said I was going to do, was I kind to everyone – things like that. These questions can be especially difficult in work environments that are not designed to uphold recovery values.
Despite all the challenges, the role can be rewarding. I have been able to open doors and invite diverse representatives of the recovery community to important meetings where expertise informs critical decision-making. Getting the right people – and the right combination of people – to the table is an art that requires intention and follow-through. And including people with lived experience as experts has been a game-changer. Demonstrating this can be as simple as setting up a workgroup participation list that omits credentials behind people’s names. Oh, this can really ruffle feathers. We know that people work hard for their PhD and other degrees but eliminating academic credentials is a way of leveling the playing field. It communicates that everyone comes to the table with equal value, no matter who they are or how they got there.
Being open about your recovery while working in government can still be difficult. There is a lot of stigma and implicit bias. Sometimes you can see it, sometimes you can feel it. Our professional language is still peppered with thoughts and assumptions that are stigmatizing and outdated. Even as the concept of recovery has gained traction in the government, attitudes from colleagues can come off as unrealistic or not fully developed and are often overly romanticized and patronizing. Because much of this happens in a work environment in which people are afraid to ask what they don’t know, I have often taken the responsibility to correct, inform, and educate.
We need people who have the skills and aptitude to take up service within government. Everything we do takes sustained effort. Look at what we have done over the past twenty years. Recovery voices are now for the most part included. There is increased awareness of harm reduction pathways. We have made progress with recovery support services, despite our concerns about areas where their authenticity and community-centeredness is compromised. Our world is better off because of our efforts. It is far from perfect, we never get 100% of what we want, but we stay at it. We stay the course. We need people in recovery who have strong recovery values and who can balance out all these challenges and stay focused on our shared goals to serve in this way.
- What would you tell young people in recovery who may be considering working within government to strengthen recovery efforts?
The recovery community and government each have cultures that often clash. To work effectively in this space as a person in recovery requires skill in working cross culturally – to find common ground and build bridges. Not everyone can do this. It is important to learn how to work like a bureaucrat without becoming one. It is easy to fall into this trap and become the barrier instead of breaking it down. Bureaucracy is a very powerful force, and it can overwhelm even the most well-intentioned advocates. This is why staying true to our values and practicing self-care is so important for those of us working in this space. If you are not careful, you can find yourself being part of the problem before you realize what has happened.
It can be so easy to lose your way if your own self-care does not come first. If you are not grounded in recovery, you can easily get lost in government. The first important consideration is to have a uncompromised practice of self-care. The second is to work government in ways that serve our community and not to end up being worked by the government.
- What are the most important values that recovering persons serving in government should consider to shape policy and strengthening recovery efforts at the state or national level?
Back in the first question, we were talking about how radical the values of the recovery community can seem to those in the larger world. So many of us in recovery value shared decision making, diversity, fairness, shared power and consensus. These ways can run contrary to the machinery of government. It can be really frustrating when you know that these values will get the best yield, but other people don’t trust or believe it. At times it feels like we are making no progress, and even that things are going backwards. The key is to stay true to those values. This is how we make incremental change. Sometimes our influence is very subtle but will take hold over time if we are persistent.
It is especially important to stay true to these values while operating in a political environment. I think many of us who have chosen this path can struggle with the political facets. It can take a lot of energy to stay true to our values while operating in the unforgiving and the sometimes-mean-spirited environment of politics. I mentioned I grew up in DC, and then moved to New York. New Yorkers are very direct people and you usually know where you stand with them. In the world of government and politics, things are more indirect: you have to read and talk between the lines. There are times when people may seem to be throwing up roadblocks when they are actually trying to help you behind the scenes. Other times, an initiative will have full support and gain momentum, only to be pulled in the final hour. The bottom line is to not become disheartened and to be as sincere as possible and authentic to yourself and the movement. It is very easy to be corrupted by power – act with integrity and don’t take yourself too seriously.
- Looking back on your career, what are you most proud of accomplishing?
The recovery movement – including recovery-oriented systems of care and peer recovery support services – is on the map in ways we have never been before. I am honored to have played a part in making that happen. It is true that we have a long way to go. You and I have spoken about a number of the problems in the way that peer services are being conceptualized and implemented. In many cases, the community elements of peer work are being undermined in favor of a much simpler and less effective annexation to the workforce. There are a lot of mistakes being made that the next generation are going to need to clean up. Yet it is also true we have people in recovery working within our care systems in roles that are based on their lived experience. This is a huge accomplishment and must be carefully guarded so that the lived experience of recovery remains key.
Systems change is hard and complicated work. Most systems are designed to self-perpetuate and create stasis to sustain its equilibrium, even when that balance is unhealthy. Let’s not forget the initial – an in some cases, ongoing – resistance to implementing a recovery-orientation and the inclusion of people with lived experience. How many years has it taken just to have these conversations out in the open? And yet there are numerous examples of federal, state, and county recovery-oriented initiatives that are promising. So, yes, our efforts have been worthy, and I have hope that the recovery community will continue to point to True North. In this regard, the next generation will achieve remarkable things if they stick to recovery values, carry forth our community goals and work to navigate these difficult waters in order to continue to expand recovery opportunities for thousands of Americans.
So over 20 years ago, a few people were bold enough to talk about highlighting recovery in a whole new way and dared to dream that the recovery community could make some positive changes in helping more people access recovery. The fundamental power of recovery is that one individual helps another, and by doing so helps heal themselves. This basic concept is one of the most powerful forces on earth. This spiritual principle is ultimately what will heal our communities, and this is the philosophy that peer support is built upon. If peer workers are not anchored in this, then it will never begin to approximate authentic peer practice. This is what so many people still don’t get: that recovery is a radical transformative process that redirects the life energy of people, families, and entire communities.
- I know that in retirement, you are focusing on your art. Art is often about advocacy. How do you see these things come together in your next chapter of life? Is your advocacy for the recovery community and LGBT community going to show up in your art?
I’ve been fortunate to live a really full life and retirement is simply a new chapter. What is essentially means is that I am liberated from having to earn a wage. A friend of mine refers to it as “going rogue.”
Except for a brief period when I was in graduate school and then started my career as a social worker and community organizer, I have always practiced my art and used it to express myself through my recovery process. My advocacy work and my art have always been connected, they come from the same place in me. One of the things I have learned as I have grown older is to stop trying to force things, to trust the process and let the universe direct the traffic. In the past, I may have focused more on the details. Now, it is about the flow. My art, my queerness and my recovery are all inseparable parts of me that focus on being authentic in the world. For me, the gift of recovery has really been about self-forgiveness, self-acceptance, and letting go of how I am perceived. I am excited about the work I am doing in the studio right now because it is about me looking the world directly in the eye and taking my place in it, without embarrassment and without apology. At least, that is the goal!
I feel good about my decision to retire. I stepped aside from a career as an artist when I answered a call to do this recovery work. After considerable prayer and meditation, I became confident that the call has shifted. Time to step aside, let others take the helm, and get back into a routine of studio practice. So I feel really confident that I got the timing right on this. And leaving a gig at the White House ain’t a bad way to cap off your career!
I have never been very good at beginnings, middles, and ends, but I am working on creating boundaries. I have also not been so good at saying “No,” either because I did not want to disappoint people or I was afraid that I would miss out on fun and opportunities. So, when asked if my work in this recovery movement stuff is over, my answer has been, “For now.” I have learned that nothing is set in stone and you never know what is around the corner.
Since my last day of work in February, I have been in the studio every day, setting up new routines and practice, and being there makes me really happy. I love having the time, space, and resources to see this new work evolve. And to answer your question, yes, there are definitely threads of social justice coursing through this work, and because I am representing no one but myself, I feel free to create work without constraint, making it as irreverent, humorous, and unrestrained as it needs to be. After years of diplomacy, it feels really liberating to unleash a set of unfiltered truths.
In closing, I’d like to remind everyone that this phase of the recovery movement began with just a few people talking about how to realize the power of the recovery community in more universal ways. It took some time for this conversation to evolve and for others to feel a part of it. Over time the spark ignited into a small flame which became a bonfire. We have yet to set the world on fire, but it is, without a doubt, coming.
The next generation has grabbed the torch and is adding new ideas and elements that are deepening the discussion, asking questions about race and inequity, arrest and incarceration, and the tensions between abstinence and harm reduction approaches. Through this exciting work and change, vigilance needs to be the watchword, along with the knowledge that we can’t give what we don’t have. We need to keep close guard on our recovery values and ensure that they are never compromised by and through our work with others. Finally, we need to keep the fitness of our recovery fresh and vital. In all the work we do in recovery advocacy and systems change, our daily spiritual practice is our most powerful tool and the compass that directs us to True North.
SMART Recovery is pleased to announce that Nora Volkow, MD will be the inaugural speaker for the new Jonathan von Breton Memorial Lecture Series, a new quarterly event featuring leaders in the recovery community.
Advancing Pragmatic Approaches to Addiction Treatment and Recovery
Wednesday, April 6th at 4:00 p.m. ET
Dr. Volkow is Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health. NIDA is the world’s largest funder of research on the health aspects of drug use and addiction. A pioneer in using brain imagery to counter myths that drug use was a moral failing, Volkow recently made a splash with an article in Health Affairs titled “Making Addiction Treatment More Realistic and Pragmatic: The Perfect Should Not Be the Enemy of the Good.” We expect her lecture to build on the themes in that article.
The Zoom event is free with registration.
Registration closes April 3rd at 11:59 p.m. ET.
The Zoom link will be emailed the week of the event.
Jonathan von Breton, CCMHC, was a longtime SMART Recovery volunteer who played a pivotal role in supporting the growth and development of the organization’s SROL online community. A Certified Clinical Mental Health Counselor, von Breton studied REBT under Albert Ellis, and was a champion of both REBT and SMART Recovery until his death after a long illness in September 2020. In 2021, the SMART Recovery USA Board of Directors established a new lecture series to recognize the significant contributions he made to the organization over more than 20 years. This lecture is the first in that series.
SMART Recovery offers effective mutual support with a self-empowering focus for those struggling with addictive behaviors, through a network of online and local in-person meetings. SMART Recovery meetings are positive, secular, and informed by empirically-based treatment methods.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
It’s not uncommon in today’s medical field to go to your family practitioner for a problem only to leave with a referral to visit a specialist rather than solve the problem right then and there. Let’s consider the value of referrals, especially when it comes to finding the best treatment program for alcohol or drug addiction.
Fellowship Hall has been providing an effective alcohol and drug treatment program for 50 years. Our program has been effective because we take the time to consult with each potential guest to discern the best possible treatment option for that individual. We receive referrals from other counselors, doctors, and other treatment centers who trust us to provide the best possible care to those who are referred. Likewise, we refer guests out to other centers and counselors we trust to provide the highest quality care for the individual, based on their specific needs.
Every individual is unique and often, there’s a complicated back-story related to substance use. Fellowship Hall works with each potential guest to determine the absolute best treatment for them – and sometimes, that means referring the individual to another treatment program that is better equipped to meet their needs.
Being referred to another treatment provider can be frustrating, particularly when you’ve done your research and selected the treatment program that you believe is the best option for you.
At Fellowship Hall, our goal is to help our guests achieve the best, most effective level of care that fits their specific needs – sometimes that means we must refer someone to another treatment center. Sometimes that means that someone is referred to Fellowship Hal from another treatment center. Referrals are an integral part of connecting individuals to effective treatment.
Why refer to a different provider? At Fellowship Hall, the most common reasons for referring an individual to another treatment facility are related to medical or behavior conditions, such as:
- The need for specialized medical care for conditions that Fellowship Hall is not equipped to treat
- Psychological conditions (eating disorder, active self-harm, etc.) which indicate the need for 24-hour monitoring
- Inability to actively participate in our treatment program due to mobility, language barriers, or other traditions that prevent active engagement in the program
Oftentimes, barriers to care can be minimized or eliminated through proper referral to a treatment center that is equipped to meet the individual’s needs. Fellowship Hall works to ensure that the receiving facility where we may refer an individual to adheres to the highest of standards.
Our role is to provide individuals with the very best care; sometimes, that means referring an individual to a treatment center that is better prepared and able to provide the best care based on the individual’s specific needs.
Guests and their family members are an integral part of their individualized treatment plan. Any questions you may have — about treatment in general and referrals in particular — should be directed to our Admissions Staff. Understanding the reasoning behind a referral offers clarity and peace of mind.
***
For more information, resources, and encouragement, “like” the Fellowship Hall Facebook page and follow us on Instagram at @FellowshipHallNC.
About Fellowship Hall
For 50 years, Fellowship Hall has been saving lives. We are a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.
As all of us at SMART Recovery celebrate Women’s History Month, it’s a wonderful opportunity to highlight the amazing leadership and accomplishments of so many talented and dedicated women in the addiction sciences, treatment, STEM, and public policy fields.
Their accomplishments are even more impressive when you consider that the playing field was not always a level one. Ivy League Universities did not admit female students until 1969. Yale didn’t grant a woman a B.A. Degree in Physics until 1978. That woman, Eileen Pollack, has written an eye-opening book on the subject of why women have traditionally been underrepresented in STEM called The Only Women in the Room.
But times have, and are, changing – and women’s leadership in the addiction and recovery fields is more evident and important than ever. Here are just a few of the amazing women working in these fields as scientists, therapists, and authors – all making substantial contributions to the quest to better understand and treat addiction.
MOLLY MAGILL, Ph.D.

Dr. Molly Magill is an Associate Professor at Brown University School of Public Health, the Director of Biostatistics at the Brown University Center for Alcohol and Addiction Studies, and an adjunct instructor at Boston College School of Social Work. One of Dr. Magill’s specialties has been adult one-to-one or group-delivered therapies based on motivational, cognitive-behavioral, SMART Recovery, and twelve-step approaches. She has generously shared her research findings with the SMART Recovery community. Watch Dr. Magill’s informative 2021 National Conference presentation analysis of new approaches to behavioral change therapies as they relate to addiction and recovery, and how SMART Recovery plays a big part in them here. She was also featured on a SMART Recovery podcast.
PROFESSOR JO NEALE

Jo Neale is Professor in Addictions Qualitative Research based within the National Addiction Centre and working across the National Institute for Health Research (NIHR) Maudsley Biomedical Research Centre at the Institute of Psychiatry, Psychology & Neuroscience, King’s College London. As such she has been deeply aligned with UK SMART Recovery for many years, and recently chaired a presentation of SMART Recovery-related research findings at the SMART Global Research Advisory Committee webinar. She has extensive research experience in several addiction-related areas, especially addiction as it relates to homelessness. Jo is also a Senior Qualitative Editor and Commissioning Editor for the international journal Addiction; a member of the editorial board of The International Journal of Drug Policy; and a member of the editorial board of Health Sociology Review. Her spirit of scientific inquiry and altruism is a true inspiration to everyone at SMART.
PATRICIA E. PENN, Ph.D.

Dr. Patricia Penn has been an Albert Ellis acolyte and loyal SMART Recovery Ambassador for decades, and recently won the 2021 SMART Recovery Science Award at our National Conference in Laurel, Maryland. While most psychologists concentrate in one area of expertise, Dr. Penn has helped patients across a broad spectrum of needs related to not just substance abuse and addiction, including family psychology, group psychotherapy, adult development & aging psychology, and cognitive & behavioral psychology. Her findings have been published in 34peer reviewed scientific journals and she is a pioneer in research about co-occurring conditions (CCs) as well as optimally empathetic and effective addiction treatment options for the LGBTQ Community. Her 2014 articleSMART Recovery®: An effective group method for co-occurring conditions in community treatment published in the Drug & Alcohol Dependence Journal, was an important step in publicly affirming that SMART is “…an effective, versatile group method for co-occurring conditions in community behavioral health treatment settings. It is useful for many types of co-occurring conditions, user friendly, easily trained, feasible, client-centered and cost-effective.”
BILLINA SHAW, M.D.

Dr. Billina Shaw is a licensed Psychiatrist and the Medical Director of Mental Health Services within the Behavioral Health Division for the Prince George’s County Health Department. A true polymath, she holds a degree in Psychology from Yale, an MD from the University of Pittsburgh School of Medicine, and a Master of Public Health from Johns Hopkins. Dr. Shaw has been a leading voice in the conversation about racial and ethnic disparities in substance use disorder treatment and care, and recently presented her findings at the 2021 SMART Recovery National Conference. Her findings were especially relevant at a public policy level given the alarming disparity in overdose fatalities between whites and people of color reported in recent years. Dr. Shaw’s work reminds us to view the causes and cures of addiction through as many lenses as possible, including and especially that of systemic racial inequality and stigmatizing language.
MAIA SZALAVITZ

The term “prolific” doesn’t even begin to describe Maia Szalavitz’s voluminous output as an author and public intellectual, especially on the topic of addiction. She has won awards from the National Institute on Drug Abuse, the Drug Policy Alliance, the American Psychological Association, and the American College of Neuropsychopharmacology for her 30 years of groundbreaking writing on addiction, neuroscience, and drug policy. She recently published a powerful op-ed article in the New York Times about efforts in Oregon to decriminalize personal-use drug possession. Maia outspokenly advocates for the increasingly accepted belief that for America to solve its overdose crisis, it must start treating addiction as a medical disorder and stop treating it as a crime. Maia recently presented her latest thoughts on addiction treatment at the 2021 SMART Recovery National Conference in a lively interview with Dr. Tom Horvath. She also just became a contributing opinion writer for the New York Times.
NORA VOLKOW, M.D.

Dr. Nora Volkow has had a significant impact on the addiction science community. She was an early pioneer in the use of brain imaging technologies to study addiction at the neurological level. Her findings, along with those of others, have helped to dispel the myth of addiction as a “moral weakness,” showing instead that addiction is a complex condition at the physiological level. It’s hard to overstate the impact of these efforts. As the current Director of the National Institute on Drug Abuse, she administers substantial funds dedicated to vital addiction science research around the world. More recently, Dr. Volkow published a provocative article in Health Affairs Magazine entitled: “Making Addiction Treatment More Realistic and Pragmatic: The Perfect Should Not Be the Enemy of the Good.” We interviewed SMART Recovery founder and former President Tom Horvath about his reaction to the article, which can be seen on SMART Recovery’s YouTube channel. We are also proud to announce that Dr. Volkow has graciously agreed to participate in SMART Recovery’s upcoming Speakers Series Webinar on April 6, 2022.
KATIE WITKIEWITZ Ph.D.

Dr. Katie Witkiewitz is a Regents’ Professor of Psychology at the University of New Mexico. The underlying theme of her research is the development of empirically based models of addiction, with an emphasis on harm reduction, recovery, and applying advanced quantitative research methods to better understand changes in alcohol and drug use behavior over time. Dr. Witkiewitz is also a licensed clinical psychologist and has worked extensively on the development and evaluation of mindfulness-based relapse prevention for addiction. Her research has been supported by grants from the National Institutes of Health, totaling nearly $40 million in research funding since 2004. To date, she has authored 5 books, written over 230 peer-reviewed publications and book chapters, and she has given over 75 presentations and invited talks. She is currently Editor of Psychology of Addictive Behaviors, Field Editor for Alcoholism: Clinical and Experimental Research, and serves on the editorial boards of Substance Use and Misuse, Alcohol and Alcoholism, and Clinical Psychological Science.
SARAH ZEMORE, Ph.D.

Dr. Sarah Zemore is a Senior Scientist at the Alcohol Research Group (ARG), Associate Director of ARG’s NIAAA-funded National Alcohol Research Center, and another amazingly eloquent, humble, and committed SMART Recovery Ambassador who won our 2019 National Conference Science Award for her research advancements in the study of the social aspects of addiction treatment and recovery. Her particular focus of study on the efficacy of mutual support groups, led to a grant from NIAAA for her to study how well SMART Recovery and several other secular programs compared to 12-Steps. Like Dr. Penn’s research finding, her results reaffirmed what many people already learned through actual experience: SMART Recovery can be an effective support system for people seeking freedom from their addictions.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

Kristal Field completed the SMART Recovery facilitator training program in 2021 and is now one class away from obtaining her masters in health administration. Facilitating a SMART Recovery meeting every week continues to teach her valuable lessons and allows her the chance to give back and serve her community. She is so grateful to have the support she needs and looks forward to having the opportunity to grow the SMART Recovery network.
Learn more about becoming a SMART volunteer
Find Kristal’s SMART Recovery meeting
Subscribe to the SMART Recovery YouTube Channel
Video storytelling is a powerful tool in recovery, and we are proud to share our SMART Recovery content free-of-charge, available anywhere, on any device. Our videos hope to inform, entertain, and inspire anyone in the recovery community.
Subscribe to our YouTube channel and be notified every time we release a new video.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

“…legitimacy is based on three things. First of all, the people who are asked to obey authority have to feel like they have a voice–that if they speak up, they will be heard. Second, the law has to be predictable. There has to be a reasonable expectation that the rules tomorrow are going to be roughly the same as the rules today. And third, the authority has to be fair. It can’t treat one group differently from another.” – Malcolm Gladwell
I found this quote above last April and half wrote this piece. One year later, it still nails what happens when systems under stress move away from their focus and only pursue narrow agendas. They get insular, reactive and autocratic. Ever shifting rules and favoritism erodes everything. They maintain the illusion of inclusion by only involving people when all the important work is done by a few favored groups. Institutions who value authentic inclusion don’t do this. Refocusing institutions who have strayed from legitimacy requires commitment to transparency and openness.
Authentic inclusion occurs without a predetermined outcome in mind. They lead to solutions founded in consensus building that could not occur in any other way. They also are more effective. Anything less reduces the legitimacy of both the process and the outcome. This leads to a system in a perpetual crisis state unable to achieve big things.
Our SUD service system is fraught with inequity. As an analogy, Walmart and local neighborhood groups do not have equal power when in disputes. Walmart ends up being treated more favorably than everyone else. They have nearly unlimited resources. They can outmaneuver all the singular voices. Individuals only have power in these dynamics when they coalesce around solutions. This also plays out in the SUD care systems across our states in resources allocation and policy development. The golden rule of “he who has the gold makes the rules” is in play. The recovery community is left out or coopted. The recovery community has no gold; our currency is community, valued when it comes together. It is the fundamental truth of our own history that outside groups profit from our division at the expense of our collective well-being. Inequity is the standard of our system and is only overcome when we stand together. We must.
These same dynamics play out on the international scale as well. This Brookings Institute article notes that economic prosperity (in terms of GDP) can become decoupled from social prosperity (in terms of well-being in thriving societies). People are getting wealthy as societies fail. Economic prosperity without social prosperity erodes nations. The recoupling dashboard, is an attempt to measure well-being beyond the GDP. Change the measure, change the outcome. Think recovery capital here. We can’t fix the SUD system without strengthening our recovery communities. This is a function of the five-year recovery paradigm, a long term wellness orientation. Not a short-term pathology focus.
Getting there is complicated for our whole system. One big barrier is our language. So much of our language around addiction and recovery is inoperable. The SUD harm reduction, treatment and recovery communities find ourselves in a situation similar to what playwright George Bernard Shaw once noted as Britain and the US as “nations separated by a common language.” We talk past each other using the same words even as those terms mean different things to each of us! We have not invested the time to develop consensus on what our common terms mean. This lack of common language also creates a barrier to thinking and acting systematically to address the common challenges we face. As a consequence, we talk past each other with little hope of deeper understanding. Our own tower of babel.
In seeking solutions, I looked towards our history. Last year, I interviewed key figures in the New Recovery Advocacy Movement (NRAM). Those interviews are HERE. It was an amazing experience, I gained a lot of insight about the movement, and I am grateful for opportunities I have to share what I have learned. The biggest takeaway for me was that several interviewers emphasized the need for broad, ongoing dialogue to develop common objectives. Not strictly facilitated groups focused on obtaining discrete goals managed by the conveners, but an authentically open process.
I am both equally encouraged and discouraged in respect to dialogue across our communities. It runs the gamut from productive conversations on difficult issues to the tired old dynamic of people waiting to pounce when their confirmation bias lights up and they move to cancel out the offender, shutting down all discourse. Creating wounds instead of healing them. Dollars are dangled to divide, more often than used in ways to bring people together. We need a system that treats all groups equally to find consensus. Strong bridges can only be built on this bedrock of legitimacy.
I see parallels to our current times and where we were 20 years ago. Things are undeniably broken. Addiction and recovery are complex issues. The power of the moment we are in is the opportunity for consensus building. It must be fixed if we are to develop and effective and cohesive care system. Such solutions take time and commitment. But as NRAM shows us, such efforts are well worth it.
What we do, or do not do will be how history remembers us.

When it comes to trying to improve access to residential rehabilitation in Scotland, one thing I’ve heard too often from doubters is: ‘there’s no evidence that rehab works’. Ten years ago I was hearing the same thing about mutual aid, which was recently (at least in terms of Alcoholics Anonymous) found to be as effective, if not more effective, than commonly delivered psychological interventions.
There are a some problems with the ‘there’s no evidence that it works’ line. The first is that even if we accept the faulty premise that there is a poor evidence base, this is often taken as evidence that rehab doesn’t work, which is illogical. The second problem is that while there is evidence, some people don’t know about it or, for a variety of reasons, choose to dismiss it. What we can say is that the evidence base is weighted towards some areas (e.g., medical interventions) at the expense of others. The third issue for me is that while we need to find ways to balance the evidence base, we will not find more evidence if we’re not looking for it.
In order to add to the evidence base, we published a paper in 2017[1], evidencing one-year outcomes following therapeutic community (TC) residential rehab in Scotland. In a review of recent literature it was good to see that our study was rated to be methodologically strong, Those patients going through TC rehab saw improvements across a range of domains. This was in keeping with previously published research.
Therapeutic community (TC) treatment is a particular type of rehab. In a TC, the community of patients itself is the main agent of change. In a highly structured programme, residents live together, share meals, participate in groups, undertake tasks within the service and share leisure activities. Lived experience in the staff team and in peer volunteers is an important component and a variety of interventions and scheduled activities offer opportunities to identify and change unhelpful thinking and behaviours, but more importantly, help to reduce psychological problems, improve social functioning and help individuals reach their goals.

Australia is producing research on residential treatment. Petra Staiger and her colleagues down under followed up 166 individuals going through TC treatment at two sites[2] and took stock of where they were nine months after discharge. They scoped out wellbeing, substance use, dependence, mental health, physical health and social functioning.
The commonest problematic substances were alcohol, cannabis, heroin and amphetamines. At baseline, participants had high levels of dependence, compared to treatment-seeking population norms. (Incidentally, we found the same in our study, in keeping with the observation that those referred to TCs have high problem severity). At baseline, individuals had very low levels of wellbeing and substantial socio-economic disadvantages.
It is critical when examining TC outcome research to understand that people accessing TC treatment tend to have more complex psychosocial concerns than people attending outpatient treatments and other shorter-term residential treatment
Petra Staiger & Colleagues,
The researchers followed up 90% of the original sample – an extremely high follow up rate for a study of this kind. At nine months post-treatment they found that 68% of individuals reported complete drug abstinence in the prior ninety days and 32% reported complete alcohol abstinence. Alcohol quantity and frequency of drinking was reduced by more than 50% and both alcohol and drug dependence scores were reduced by over 60%. Wellbeing scores doubled and psychiatric severity scores halved. Longer stays in the TC had better outcomes.
This study chimes with what we found in our outcome study from TC treatment in Scotland – high baseline problem severity but significant improvements in a range of measures one year after treatment. There are good reasons to be positive about the impact of rehab and plenty of evidence with which to challenge the naysayers.

Having said that, and while very welcome, such findings need to be seen in the context of a wider treatment system where a full menu of options is available. Not only that, but the components of the treatment system need to be linked in a way that makes navigation between them simple and as safe as possible. When rehab is seen as separate from mainstream treatment – a remote silo – then the chances of individuals getting there easily is reduced and the risks are likely to be higher. We need an integrated system of care and I hope we are moving towards that here. As we can see, according to the evidence, there are good reasons to make rehab an integral part of treatment systems.
Based on their methodology, high follow-up rates and outcomes, the authors conclude:
The findings reported can be viewed with confidence and are likely to generalise to the TCs within Australia and beyond.
Continue the discussion on Twitter @DocDavidM
Main photo credit: Nazarkru@istockphoto under license
[1] Rome AM, McCartney D, Best D & Rush R (2017) Changes in Substance Use and Risk Behaviors One Year After Treatment: Outcomes Associated with a Quasi-Residential Rehabilitation Service for Alcohol and Drug Users in Edinburgh, Journal of Groups in Addiction & Recovery, 12:2-3, 86-98,
[2] Staiger PK, Liknaitzky P, Lake AJ, Gruenert S. Longitudinal Substance Use and Biopsychosocial Outcomes Following Therapeutic Community Treatment for Substance Dependence. Journal of Clinical Medicine. 2020; 9(1):118.

Peer-to-peer fundraising has proven to be a fun, engaging, and effective way for nonprofits to raise funds for the vital work they do in service of their communities. Now SMART Recovery is proud to roll out its very own TAKE ON ADDICTION campaign starting April 1st!
This is a first-of-its-kind global initiative to Smash the Stigma associated with addiction and inspire people everywhere to confidently step forward, access SMART Recovery’s free tools and mutual support meetings, and truly get the help they need.
As a vital member of the SMART Recovery community, YOU understand more than anyone how important these efforts are. We invite you to take part. Simply sign up here to set up your personalized online profile, then set daily or weekly goals to walk, run, cycle, or choose your own activity to raise funds for the campaign.
Create a team! Invite your friends and colleagues to join it or invite them to start their own teams!
Your fundraising efforts this April will not only help you get really fit, but also push SMART Recovery ever closer to its ultimate goal of having everyone, everywhere, live Life Beyond Addiction.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
In the first part of this article, I’ll note one particular barrier I have heard expressed about the idea of changing an addiction treatment campus to “tobacco-free” or to the idea of a tobacco-free model of care. And then I’ll discuss a few responses to that barrier.
In the second part of the article, I’ll provide a list of some possible reasons why 480,000 deaths1 a year due to smoking don’t get our attention and don’t cause us to adopt a smoke-free model of addiction treatment.
PART 1: One particular barrier, and some responses to that barrier.
One Particular Barrier
The organization where I work made the switch2 to a tobacco-free campus back in 2013. From time to time after we made that change, I’ve been asked an interesting question. The question comes in a few different versions, and it points to one particular barrier against making the change to a tobacco-free addiction treatment method and campus.
Here are the two most common versions of the question:
- “Isn’t it the person’s right to smoke cigarettes?”
- “But isn’t smoking cigarettes a human right?”
Interestingly, every time I have been asked any version of this question it has been asked of me by people with clinical careers in community agencies providing addiction treatment and mental health counseling services or related human service help.
On the topic of tobacco, it seems as if the professional part of our field knows the right answer but keeps walking in the wrong direction.

I wanted to share a few of my responses to that question, in no particular order.
Response #1: Treating One Addiction While Ignoring Another
In this reply I ask what it even means to claim to provide “addiction treatment” and yet treat one addiction while ignoring another.
One question of my own that I’ve used as a probe of our intent as addiction professionals is:
“If a person we treated for alcoholism dies of emphysema due to continuing smoking cigarettes, did we really treat their disease, or just an alcohol use disorder?”

We all know the standard response to that challenge is, “We don’t ignore cigarette smoking”. And in this context the other response that “…addiction isn’t really a disease…” is outside the meaning of the question.
Rather than contend with the point of my probe, some will state their…
- use of motivational interviewing, NRT’s, patient education, and a tobacco-specific group; or
- inclusion of tobacco as a part of the patient’s clinical assignments or homework.
But I’d like to state that if it was cocaine or methamphetamine the patient was smoking instead of cigarettes, we would likely not be so lackadaisical or cavalier.
Response #2: Do No Harm
Another response I give at times is one concerning “Do no harm.”
Addiction professionals with clinical credentials have a clinical duty to those we serve. Among those duties we are to:
- Not do harm to those we serve
- Provide an atmosphere or environment of care that does not harm any patient
Even if it was the human right of one person to smoke cigarettes, would that one person’s right within their personal space and life remove our responsibility to anyone else or everyone else we serve in our clinical setting? Would we be willing to harm all within our setting for the sake of the freedom of one?
My current view of this challenge is that it pits the personal freedom of a smoker against the patient rights of someone else who is seeking services. That is, a smoker does have a personal freedom to smoke. But a different person seeking services in the same setting has a patient right to a smoke-free environment. My view is that at an SUD treatment providing organization, the freedom of one person to smoke ends at the line of the rights of others to access care in a smoke-free environment.
Response #3: The Right to Slowly Die
I usually don’t include any part of this third possible reply, but I’ll present it here regardless.
When I include this, I start by acknowledging the value of the question concerning the individual and their human right to smoke cigarettes. I state that the question is simple, good, and powerful – at the surface level. And I affirm that yes, it is the person’s human right to smoke cigarettes.
And then I introduce the idea that there are potentially complicating matters of law, ethics, and morals. And that similarly, these matters can be phrased as questions as well.
Examples within each category follow.
- Law: Is the person legally permitted to purchase, possess, and smoke cigarettes, or are they under-age?
- Ethics: Has the patient been asked to sign a “Do Not Resuscitate” order in case of heart attack or stroke while they continue to smoke under our care? Have we offered transfer to an “Addiction Hospice” type of SUD care if such a program exists nearby, where dying slowly is the pre-determined plan? Do we realize the implications of the care we do provide and do not provide, and discuss those plainly in our informed consent?
- Morals: Do we offer our staff the standard “Exception From Care” option on smoking-related tasks, and make the related reasonable accommodations? I remind them that “exception from care” is a standard in place so that staff are not required to violate their conscience or personal sense of morality. And I link this standard to the topic of tobacco-free treatment by asking if staff have the Exception From Care option on tasks that require them to actively support or under-treat tobacco smoking as a job function while they are working in addiction treatment?
More to the point, does the patient have a right to die slowly while we watch?
- If it was any other disease, we would do a wellness check, or call an ambulance, or have the person who is allowing themselves to die involuntarily committed as a danger to themselves.
Response #4: Choosing a Human Right or Enacting a Loss of Control?
In this response I note that while picking up their first cigarette ever, the person might have been exercising a choice to smoke.
But to the extent the person now:
- has a persistent desire or inability to cut down or quit smoking
- experiences cravings and urges to smoke
- is losing role function or areas of life due to use
- experiences withdrawal when they don’t smoke…

…it might be that they are not choosing freely but are experiencing a loss of control. And personally, I differentiate loss of control from the notion of a personal freedom.
PART 2: Some possible reasons 480,000 deaths per year due to smoking don’t get our attention or lead to change.
To develop a partial list of some possible reasons our field does not adopt a smoke-free model of treatment, I’ve borrowed some notions from an article3 and applied them to this topic. Below is a list the reader could review toward identifying barriers to this change.
Possibilities might include:
- Allowing smoking is a “residue of the somatic process” still present in organizational leaders, who are current or former smokers.
- Leaders in addiction treatment providing organizations are relatively unaware of how they look on this topic from the outside.
- Leaders in addiction treatment organizations do not discuss their lack of change on this topic in a meaningful way with those outside their organization and prefer to keep it unacknowledged on the social dimension.
- Leaders in addiction treatment organizations take their cues from other leaders in the field; they see other leaders are doing nothing, assume those leaders are thoughtful and intentional, and thus also do nothing.
- Workers and leaders in addiction treatment organizations have a special hindrance that if not present would allow them to obtain a true knowledge of this topic.
- Workers and leaders in addiction treatment organizations, seeking to remain comfortable, enact the process of addiction by allowing it in others, disavow that fact, and attend only to their work tasks.
- When the voice that emanates from within shines light on this matter, that voice is censored, serving to keep the thing out of awareness.
- The charge for personal wellbeing, within organizational leaders, is neither held at the whole person level nor allowed to work progressively over time – but is merely localized within them; thus, their leadership in their own organization is localized by topic.
- Fear of the smoke-free idea, based on fear of the image others would see if the idea was adopted, based on fear of presenting that new and different way of operating to the world at large – and doing passionate self-preservation instead.
- Understanding the smoke-free idea, but not feeling the idea.
- Maintaining the topic at the border between acknowledgment and unawareness.
- The choice to not acknowledge smoking and to take on the problems associated with that choice is preferred over the problems associated with the choice of addressing smoking.
- Maintaining treatment as usual – in its service as a phobic outer structure for an unacknowledged worry.
- The deep knowing that the smoke free approach is the best in reality – but that knowledge is exempted from consideration given the timeless lessons that have taught us avoidance.
- A certain inherited view of making this change, and long ago leaving the idea of this change discarded and unserviceable.
- Adhering to the precious approach with a stilted explanation that does not permit this change.
- Isolation from those that discuss this change with words rather than with emotions and the ideas related to those emotions.
Conclusion: Raising Doubts About Not Changing
We learn in motivational interviewing that raising doubts about the lack of change can help tip the decisional balance. And we learn that providing information can help accomplish that some of the time. Thus, I’ll conclude by providing some information and related resources.
“Tobacco use is the leading preventable cause of death in the United States”.4
“Cigarette smoking causes about one of every five deaths in the United States each year.”4
Smoking is associated with 5 times the risk of relapse 3 years later.5
Severity of nicotine dependence is associated with higher craving in alcohol-dependent patients. This suggests shared pathophysiological mechanisms in alcohol craving and nicotine dependence.6
Tobacco use is correlated with relapse. Addressing tobacco in treatment improves outcomes.7
So, what are some reasons to address tobacco use in addiction treatment settings? And why change to a tobacco-free model of addiction treatment?
- High rates of tobacco use in individuals being treated for other substance use disorders
- Greater morbidity and mortality in individuals who use tobacco and other substances
- Higher relapse rates in patients who do not stop using tobacco
- Patient and staff exposure to second-hand smoke
- Increased risk of new tobacco use, in non-tobacco using patients
In our organizational change process, we went through stages of change over a series of years as an organization. Eventually, we made the decision, including a decision at the emotional level, to get in alignment with both our own values and the evidence – to treat the core disease.
And in so doing, we recognized that cessation might be little more than an attempt to control one’s tobacco use disorder (and that quitting would be diagnostic, not prognostic). And so, we decided to not use a cessation framework, but to use a wellbeing or recovery framework instead.
References
The references are provided in a clickable format for your convenience.
3 Freud, S. (1915). The Unconscious. SE14: 159-215.
4 CDC Tobacco-Related Mortality
7 Stuyt, E. B. (2015). Enforced Abstinence from Tobacco During In-Patient Dual-Diagnosis Treatment Improves Substance Abuse Treatment Outcomes in Smokers. The American Journal on Addictions. 24(3): 252-257.
Recommended Reading
Fiore, M. C., Jaén, C. R., Baker, T. B., et al. (2008). Treating Tobacco Use and Dependence: 2008 Update. Rockville, Md.: U.S. Department of Health and Human Services, Public Health Service.
Goodheart, C. D. & Lansing, M. H. (1997). Treating People With Chronic Disease: A Psychological Guide. American Psychological Association.
Hilton T. F. & White W. L. (2013). Why Does the Addiction Treatment Field Continue to Tolerate Smoking Instead of Treating It? Counselor. 14:34-7.
Knudsen, H. K. & White W. L. (2012). Smoking Cessation Services in Addiction Treatment: Challenges for Organizations and the Counseling Workforce. Counselor. 13:10-4.
McKelvey, K., Thrul, J. & Ramo, D. (2017). Impact of Quitting Smoking and Smoking Cessation Treatment on Substance Use Outcomes: An updated and narrative review. Addictive Behaviors. 65:161-170.
U.S. Department of Health and Human Services. (2014). The Health Consequences of Smoking – 50 Years of Progress. A Report of the Surgeon General. Atlanta: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.

Alex received his first video game station at the age of two. His love and eventual addiction to video gaming continued throughout his life. It wasn’t until recently that Alex found SMART Recovery, and has made positive changes to his life and began managing his problematic behavior.
In this interview, Alex talks about:
- His dad buying him a VecTrexat two years old
- The progression of gaming systems and how the technology over time
- The “water cooler” conversations around new video games
- First realizing that there was an issue with gaming when he didn’t “grow out of it”
- The “Just Say No to Drugs” PSAs being counterproductive in video games
- The opportunity cost of continuing to play video games
- Video gaming addiction characteristics
- Trying other recovery programs, then finding SMART
- The ways SMART talks about addiction and the nuances for helping each person differently
- How the pandemic affected his addiction
- Knowing he can’t keep throwing his life away
Additional resources:
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!