Bill White recently wrote a powerful post about the intersection of recovery, character, and activism. First, on character as an essential element of recovery advocacy:
What is the role of character reconstruction in addiction recovery? In recovery activism? I have repeatedly returned to these questions over the course of my adult life, especially as young recovery advocates sought my guidance on how to best use their lived experience as a catalyst for social change. Effective recovery advocacy and peer recovery support depend on the scope and depth of one’s knowledge and skills, but equally important is this dimension of personal character.
He goes on to explain that advocacy founded on personal character requires a personal mission and code:
The challenge in recovery is how to rebuild a name (character) ravaged by the addiction experience. The challenge in recovery advocacy is how to use the fruits of that character reconstruction as a fulcrum for one’s service to others. As Burroughs suggests, service to one’s cause requires a foundation of personal integrity. That, in turn, requires a personal mission/vision (What am I here to achieve?) and a personal code (What are the values and personal code that will guide my journey toward that goal?)
Bill shared his own mission/vision and code, which I strongly recommend you read and reflect upon. It includes maintaining his own recovery, emphasizes listening to others, seeking to understand people who offend him, humility, and supporting the freedom of the people he seeks to serve.
He follows his own code with this statement:
Such an actionable set of values constitutes the building blocks of character. It enriches the recovery experience, quiets the childish attention-seeking of the self-absorbed ego, and enables compassion and care for others.
The post is worth reading, contemplating, and re-reading.

Sarah Levin is the founder of Secular Strategies. She is also a lobbyist and coalition builder. Sarah has made it her life’s work to fight for legislation protecting secular points of view.
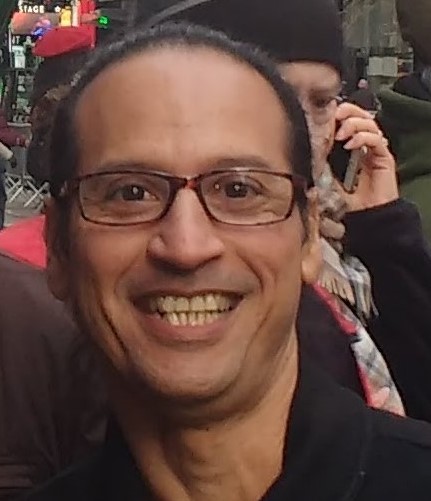
Gerardo (Gee) Matamoros is a SMART Regional Coordinator, president of the SMART NYC Board, and self-described newfound activist. He is impacting his community through his passion and dedication to ensuring SMART is an option for everyone in recovery.
In this podcast, they talk about:
- Sarah growing up in a political family that loved to talk about religion and politics at the kitchen table
- Sarah being introduced to SMART when she worked for the Secular Coalition for America
- Being the engine of the secular movement
- Gee grew up in different countries and came to the US for college
- Gee’s stint with “naughty” substances and finding SMART
- What brought Sarah and Gee together
- Advocating for separation of church and state and evidence-based policy
- Explaining to law makers why Medically Assisted Treatment (MAT) should be supported in recovery
- Ending the stigma of addiction for people in recovery
- The First Amendment cases that protect choice in recovery pathways
- Shifting the burden to the courts to ensure secular recovery options are given to people
- Gee’s outreach and awareness efforts in NYC
- Newfound energy in rallying people to get involved in SMART’s legislative changes
- Why it’s important to learn the ecosystem of decision makers in your community and make SMART known
- Telling your story because your voice matters to lawmakers at all levels
Additional resources:
Click here to find all of SMART Recovery’s podcasts
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

Pete Rubinas found SMART Recovery when he observed someone close to him transforming their life using SMART tools and techniques. That led Pete to examine his own relationship with alcohol, and he decided to build a new balanced alcohol-free life without it with the help of fellow meeting participants.
As part of giving back to a program that helped him live his best life, Pete started facilitating regular SMART Recovery meetings before helping to found the first local SMART Family & Friends meetings in the Triangle region of North Carolina. He’s gone on to become the SMART Regional Coordinator for North Carolina, supporting other facilitators around the state as they strive to provide compassionate support to those struggling with an addictive behavior.
Learn more about becoming a SMART volunteer.
Subscribe to the SMART Recovery YouTube Channel
Video storytelling is a powerful tool in recovery, and we are proud to share our SMART Recovery content free-of-charge, available anywhere, on any device. Our videos hope to inform, entertain, and inspire anyone in the recovery community.
Subscribe to our YouTube channel and be notified every time we release a new video.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

When the news of Scotland’s 2020 alcohol-specific deaths – all 1190 of them – was published last month, I was fascinated to compare the reaction in the press, TV and social media to the respective reaction after the publication of the drug deaths. Our ‘other’ drug deaths, quite rightly, provoked outrage, grief and calls for change. To me the response to the alcohol deaths seemed like a whimper rather than the bang such loss deserves.
Beyond the terrible impact of those deaths is the astounding cost of alcohol harms to the Scottish economy. In 2010, the Scottish Government estimated that the cost of excessive drinking here is around £3.6 billion when social, criminal justice and health factors are considered. The fallout in families and communities is considerable.
When we were exploring access problems to residential rehabilitation in Scotland, the Residential Rehabilitation Working Group did not find any evidence that access for alcohol problems was any better than for drug problems, yet there has been little energy spent on trying to increase access for this group.
Given that there was a 17% year on year increase in fatalities and that the number of alcohol-specific deaths is a significant underestimate of deaths in which alcohol plays a part, I wondered in a tweet why there was a more muted reaction to the alcohol deaths than to the drug deaths. This touched a nerve it seems. A lot of responses were generated and I wanted to share some of the themes here.
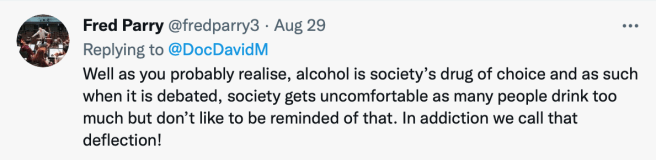
Fred Parry, who recently made a poignant plea for more action on alcohol addiction in the Ferret makes the salient observation that there may be a degree of denial going on because alcohol is society’s ‘drug of choice’. Several commentators picked this theme up including Steven R.
The way alcohol is seen and the allowances made for it are relevant to this debate:
I am pretty much in agreement with Emma Rogan:
And do the press collude in keeping attention deflected? Bobby Smith thinks so:
There was emphasis on the contrast of the legal drug alcohol with illicit drugs, perhaps meaning we pay less attention. Perhaps too, the illicit nature of other drugs creates a glamour/mystery which causes more of a splash. My colleague, Garret McGovern picks this up, also :
The idea of underinvestment in alcohol services was challenged by Andrew McAuley:
It’s true a lot of effort has gone into policy – we have national minimum unit pricing and alcohol brief interventions, but what about treatment? Peter Rice had a different perspective:
This raised for me the unwelcome thought: what if our understandable emphasis on tackling drug deaths was having the unintended consequence of our neglecting of alcohol deaths?
Perhaps the ferocity and immediacy of other drug harms are relevant:

And does tax revenue and lobbying from the alcohol industry have a part to play in our dulled response?
I wonder too if part of the problem is the swing of the pendulum. We have trouble with multitasking – at points in the past, the emphasis has been on alcohol. At the moment it’s more on other drugs – perhaps it will swing back, though what we really need is a mid position where we give alcohol problems and their prevention, harm reduction and treatment the same priority as other drugs. You can see many more comments here.
For the moment though, for the sake of all those suffering and dying prematurely – and their families, I think we need not the whimper we got in response to alcohol deaths but a very loud bang instead.
Continue the discussion on Twitter @DocDavidM
Note: I’ve not sought permission to publish these tweets as they are already published in the public record, – but if anyone would like me to remove their comment, please let me know. Thanks to all who took time to comment on the Twitter thread.
Join SMART Recovery on September 24-26 for our first-ever, nationwide Pathways to Recovery walk. This virtual event is sure to provide a day of reflection, exercise, and fun. In addition, your fundraising efforts will enable us to help more people who are on the path to recovery find life beyond addiction.
There is no RIGHT way to recover. Individuals who choose their own pathways to recovery are more likely to move from a life of substance misuse and self-harm to a life of positive self-regard and willingness to change. Supporting and celebrating this idea of multiple pathways to recovery is what our new event, Pathways to Recovery, is all about.
About the Pathways Walk
- Choose your own 1+ mile path
- Walk anytime on the weekend of September 24-26
- Participate alone or with your family and friends
- Take pictures with the hashtags #multiplepathways and #SMARTRecovery, and tag SMART Recovery on our various social media platforms
How to Participate
REGISTER
Register by September 23 to take part in our virtual Pathway to Recovery walk, the weekend of September 24-26.
SUPPORT A FUNDRAISER
Donate to a personal fundraising page to support the “Pathway to Recovery” event.
PAVE THE PATH
Help us pave a virtual path to recovery! Buy a virtual brick in honor or memory of a loved one or to honor a hero in your recovery journey.
Questions, please contact giving@smartrecovery.org
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
When the Doctor Is In… Treatment: When Helpers Need Help

What happens when those who treat, support, heal, or educate need treatment, support, healing, and education of their own? This is a question that many professionals are negotiating when they enter treatment for their own experience of addiction disease. As we know, addiction disease does not discriminate. It is an equal opportunity illness which means that anyone— regardless of his or her professional successes— is susceptible to its emotional, physical and spiritual destruction. In working with lawyers, physicians, pharmacists, physicians’ assistants, counselors, executives, and educators there are some issues that arise for professionals that are (but don’t have to be) unique.
Look at what I have accomplished, how could I possibly be addicted?
For many professionals, the dissonance created from a lifetime of academic and professional successes in the face of addiction disease can be difficult to negotiate. At times, the unmanageability of addiction is glaringly obvious and has spread to a professional’s work life. This can include legal problems, complaints filed with the professional’s board, or job loss or demotion. In other circumstances, the professional has been able to keep his or her work life largely intact. As professionals begin to expand their awareness of the breadth of their lives to include relationships, emotional and spiritual worlds, the impact of their addictive process becomes clear. Often professionals find that as they tend to the disruption addiction has created in these areas of their lives, their professional successes could not ease the emotional and spiritual wounds they have been carrying since long before they were addicted. By addressing this relational and emotional unmanageability, professionals find more meaningful and fulfilling relationships with patients, clients, colleagues, and family members that are mutually supportive of one another in both recovery and beyond.
How am I supposed to be the patient or client?
The old adage that “doctors (or nurses and healthcare professionals) make the worst patients,” holds a kernel of truth. As professionals make the transition from offering direction, care and/or advice, to being the recipient of such direction and care, it can naturally be a jarring and uncomfortable transition. Learning how to give oneself permission to not know and to be helped and cared for can offer professionals much needed relief from the pressure of high stress expectations. Allowing oneself to be vulnerable to support gives professionals permission to be human when often their professions demand perfection. Many times, professionals find that they have looked to alcohol and/or drugs to provide them with the exact relief that is found through the acceptance of the support available in a treatment and recovery environment.
What if I see a patient or client in a meeting?
The more accurate question is not “if” but “when.” An entire essay could be written about all of the “what if” scenarios that can occur at Twelve Step recovery meetings. Shame says that patients and clients will “think less of me, avoid me, or stop seeing me if they see me at a meeting.” The reality is that the opposite is more often the experience. Patients and clients feel understood, seen, and heard by professionals with whom they can relate and see as equals. Many recovering people seek out professionals who understand addiction and the importance of recovery, as they feel safe to share openly about their history.
How can I fit meetings into my work schedule – especially when I have been gone for so long?
This issue often involves a significant paradigm shift for professionals whose priority has been work and career— often at the cost of self-care and personal relationships. Many times, organizational and professional expectations compound this belief to the detriment of its employees. This reprioritizing can begin through external support (monitoring entities or restricted practice) and eventually become internalized to support long-term recovery efforts. Professionals, like others in recovery, can start with the acceptance that because of active involvement in recovery, aftercare and individual counseling, meetings, connections to others in recovery, a full life is available. It is because of the hard work that occurs during treatment that continuing to be in one’s chosen field is possible. By tending to recovery first, professionals are able to teach colleagues, patients, and mentors about the need to take care of self, first… and then others.
How do I talk with my colleagues about where I have been?
It depends. Working professionals returning to work after a lengthy and/or unexpected absence can feel internal pressure to either over-disclose or simply avoid the topic all together. It seems that the closeness and safety of the relationship really dictates the nature of the disclosure. Professionals who are involved with monitoring boards have access to a wealth of guidance and support that can be helpful in negotiating these conversations. At times, mentors who are also in recovery, are available to help professionals as they transition back to home and work, from treatment. This kind of peer support is invaluable. Many professionals find enormous and unconditional support from close co-workers and colleagues who have been gravely concerned unbeknownst to the professional in treatment. In other circumstances, keeping any discussion at all short and vague is best. For colleagues, asking “How are things going for you since I last saw you?” is always a good option as most people are happy to talk about themselves.
The path of recovery.
While some of the issues that professionals address in treatment are unique to their high pressure, success-driven careers, the solution is the same as for those who may be unemployed, under-employed or have low-stress, easy-going jobs: connection and vulnerability. These two experiences offer all recovering people a safe harbor to find self-acceptance, community, and humanness. A place to create a full and fulfilling life that offers joy and hope to all of those who seek it.
Contributed by Mahala Motzny, Counselor
About Fellowship Hall
Fellowship Hall is a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.
A few days ago David McCartney posted an interesting piece titled “Choice in addiction treatment.”
That post got me recollecting about clinical practices in our outpatient methadone maintenance program that I thought I would briefly share – in case this historical information is somehow helpful or interesting to someone.
Our methadone maintenance program began operation in either 1968 or 1969. I was told a first-hand story of its founding, but don’t remember the year. (By the way, the first journal article describing methadone maintenance as a clinical practice was published in 1965, so those were some “early adopters” indeed).
When I began work in the 12 month residential drug-free therapeutic community in 1989, the methadone maintenance program was operated in the first few offices in the front of that residential program. And the two programs shared the same nursing and counseling staff. Believe it or not but when I started there the first nurse (RN) approved by the State to dispense methadone (who began work in 68/69), was still working in that program. And more amazingly, she continued to work there for at least my first decade working in that program.
Upon my arrival in 1989, our methadone maintenance program practices included:
- Patient limit of 50 total people on the program
- No minimum or maximum dose limit
- No minimum or maximum time on the program
- 7 day RN coverage on-site, 365 days per year, providing medication dispensing
- Phase system based on developmental milestones of improvement (stabilization, diminishment of clinically relevant problems, gains in practical life goals, sustainability of improved quality of life, etc.)
- Use of substances other than opioids was addressed according to clinical relevance (e.g. a moderate to severe problem in its own right; or use of a substance class that was not another use disorder, but represented a general relapse process; or seemingly no real relevance at all).
Later in my time there, our agency undertook a multi-year (1998-2007) change-project across the dozens of programs in our organization. That effort was called the Behavioral Health Recovery Management (BHRM) Project. We used the BHRM Principles to direct specific changes. At other times we would pick a Principle and use that Principle as a goal toward which we would make many changes at once or in a row.
During those years we made vast changes to policies and procedures at both the organizational and program levels. We went as far as wholesale elimination of the entire clinical guts of some programs and total replacement of their methods with new practices.
For the methadone maintenance program we adopted changes that included:
- Budgeting 10-15 blood draws per year. We did these to check the circulating methadone level both one hour before and four hours after, one dose. We used these levels to see if the patient’s body was metabolizing the medication properly (rather than us not believing the patient that their medication was not “holding” them).
- Viewing an addiction to another drug class (like alcohol, for example) as a co-occurring disorder. We would eventually refer the patient up to a short or long term residential level of care if necessary. But we would continue their methadone maintenance while they were there if they wanted to, and it was not clinically contra-indicated. In doing so we would hold their slot on the methadone program if they wanted to stay on the medication and continue in outpatient methadone maintenance after completing residential treatment.
- Adding a “Family Night With the Doc” quarterly. We had patients invite and bring their family members at least once, but it was optional after the first time. The night included elaborate snacks, beverages and desserts in a casual but organized format. The program physician would share some brief educational comments, take questions, and respond to any discussion topics raised by the family members and the patients in an open format.
- Having our patients continue to come to the very same group therapy for their entire first year off of methadone – if they chose to taper off the medication.
- Obtaining methadone dosing privileges at our County Jail. Our nurse would personally bring them an off-site dose each day, with the idea you would naturally stay on the program if you wanted to when released.
- Obtaining methadone dosing privileges inside all of our own drug-free short and long-term residential addiction treatment programs. Our nurse would personally bring them an off-site dose each day with the idea you would naturally stay on the program if you wanted to when you completed residential treatment
- Buying the starter kit, and providing free use of a large comfortable room in our program, during off-hours (no groups happening), for the patients to start and hold meetings of Methadone Anonymous. I personally worked with our patients on this idea for four years before the idea “took” and they started the meetings. I didn’t think it would take that long, but we just kept encouraging it. We knew that they needed to start and run it, as service, if they chose to. And that if we started it or controlled it that it wouldn’t work and wouldn’t last.
- Finding out which 12 step, faith-based, and other meetings in town (very specific days/times of certain meetings) were friendly toward the idea of methadone maintenance patients being “in recovery” and also allowing them to share – if they fit into the meeting and followed the guidance of the Chair. We tended to suggest they attend these meetings
- Finding out which 12 step, faith-based, and other meetings in town were openly hostile to that, and tended to suggest they avoid those meetings.
- Adding patient education and counseling that incorporated basic principles and practices from the Advocates for the Integration of Recovery and Methadone (AFIRM).
Some of our ideas and efforts made it into print. And so did some extensions of these efforts.
Suggested Reading
Hentoff, N. (1968). A Doctor Among the Addicts. Rand McNally & Co
Strain, E. C. & Stitzer, M. L. (Eds.). (1999). Methadone Treatment for Opioid Dependence.
We are pleased to announce the release of our newest Tips & Tools for Recovery that Works! video DIBs.
We all hold beliefs which guide our actions and influence our feelings. But some of these beliefs may be irrational. And many irrational beliefs may be actually harmful to our recovery.
The SMART Recovery tool DIBs stands for disputing irrational beliefs. It’s a system for breaking down why a belief may be irrational and then applying a systematic approach to come up with a more rational belief to help us along in recovery.
Subscribe to the SMART Recovery YouTube Channel
Video storytelling is a powerful tool in recovery, and we are proud to share our SMART Recovery content free-of-charge, available anywhere, on any device. Our videos hope to inform, entertain, and inspire anyone in the recovery community.
Subscribe to our YouTube channel and be notified every time we release a new video.
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments
we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
Leading the Future of Recovery
Saturday, October 23, 2021
SMART Recovery is a global movement of self-empowering addiction recovery mutual support meetings. We, along with many others, are truly leading the future of recovery and we want you to join us in our mission.
Join us at the 2021 SMART Recovery National Conference to hear from members of the SMART Recovery community, addiction recovery experts, and industry leaders. Learn about the current state of addiction recovery, what the future landscape looks like, and how SMART intends to be involved in the solution.
Conference Details:
- Time: 9:00 a.m. — 5:00 p.m. ET
- Location: This is a hybrid conference, with most attendees participating via livestream. Limited in-person tickets are available. The event is being held at the DoubleTree by Hilton in Laurel, MD.
- Cost: General Attendees: $50, Treatment Professionals (6 CEU credits): $90
- Register by Text: TEXT 2021SMARTCON to 41444
- Register Online: www.smartrecovery.org/2021conference
Conference agenda, speakers, sponsorship opportunities, and more can be found at www.smartrecovery.org/2021conference.
Contact conference@smartrecovery.org for more details.
Thank you to our sponsors
Level One
Level Two
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

The other day, as I was going through social media, I saw a friend talking about being in a store when an alarm went off when what he had purchased set off an anti-theft device. He spoke about what a great feeling it was to stop and wait for a clerk to deal with the situation and how it differed from his active addiction experience. He noted it was far different because he shoplifted while in the grips of his addiction when he engaged in illegal conduct to support his use. He was not glorifying it, and the focus of what he said was about how positive recovery is for him because he no longer does those things. Someone told him on his thread that talking about his consequences in that way was wrong.
I am seeing this form of social media censoring occurring more frequently as tribalism seems to be taking over social discourse in our society, not just in the addiction and recovery realm. But it is particularly dangerous for the recovery community, who have long benefited from open discourse with a focus on broad consensus building. Ours is a community with many strong opinions. We achieve great things when we find and work on areas of common concern. The dangers of homogenizing our stories was a topic last year in this paper on the topic of recovery storytelling. It was an honor to work with Bill White and Danielle Tarino on a paper focused on opening up dialogue on personal privacy and public recovery advocacy focused on the ethics of sharing our stories and their value to the new recovery advocacy movement.
What caught my eye in reading the post, was that the individual was being chastised by another person for talking about addiction in ways told that person’s uncomfortable individual truth, even as they were emphasizing the benefits of recovery. The sense is that even acknowledging things within the common knowledge of our society like criminal behavior in active use might reinforce stigmatized attitudes about people who experience an addiction. This moves us towards an unrealistic, homogenized version of addiction and recovery that is not actually reflective of what a severe substance use condition looks like. The unvarnished truth is that addiction often leads people to do things outside of their own codes of conduct, even illegal and dangerous things. It was true for me; it is true for the vast majority of us with severe substance use disorders. There is a long list of things that I did while addicted that I would not do now with a fully functioning brain.
Addiction is a condition of the brain, particularly the areas of the brain associated with executive function. The reasoning areas. Addiction also impacts the limbic system, the area of the brain that deals with base functions, the four Fs of evolutionary drive. For me, it was like the area of the brain in charge of reasoning between right and wrong was the quietest of whispers and the base function area of the brain that wanted the numbing sensation of the drug was shouting in my ear to do whatever it took to use drugs and ignore everything else between myself and the drug. As my brain healed, this reversed, and the executive function regions became much louder, the limbic system a quiet whisper. I have spoken about this dynamic with many persons who have experienced addiction over the years and in general that seem to understand this as similar to their own experience. It is common for those of us with severe forms of addiction. It is frightening to know from a lived experience what happens to volition in the grips of addiction, trust me on this.
What bothered me most about reading the exchange is that there is an increasing tendency to admonish anyone who acknowledges the things that we all commonly know about addiction. That drug use can lead to addiction and by extension, as addiction takes hold in the brain, it can cause people to do things that they would not otherwise do. I stay in recovery for two fundamental reasons. The first of which is that I can live the life I want free of drugs and alcohol. Moderation is not a choice for a person like me with a severe form of the condition. My life is much better this way! The second reason is that I am reasonably sure from what I can see in the literature and from experiences I see around me that for a person with a severe substance use disorder like me, use leads down a path where my very ability to act on my own volition become uncertain as addiction hijacks the brain. I have a responsibility to myself and others around me not to allow that to happen. Like thousands of others with severe substance use conditions, I don’t use drugs, so my brain stays functional and I remain a fully functional, productive citizen.
In some work with colleagues, I am doing currently on stigma, the topic of this post is one that we are having a fair amount of productive dialogue on. Stigma against addiction, drug users and people in recovery is a profound problem, one we are focused on addressing with hard data in ways that have not been done before. It is an important project. In that survey of thousands of Americans, 71% of respondents believed that society at large considers individuals who use drugs problematically to be outcasts or non-community members. Views on people in recovery were just as abysmal. How can one get help if society sees you as an outcast? The magnitude is immense, according the 2016 Surgeon General’s Report on Alcohol, Drugs, and Health 20.8 million people (7.8 percent of the population) met the diagnostic criteria for a substance use disorder in 2015. We need to change attitudes, be seen as human and treated as such. That is not where we are right now, not anywhere close. The perception in the general public is that roughly only one in three Americans see me as a full person because of my addiction and recovery status.
We must ensure that once addicted, a person is treated with respect and offered compassionate help. We don’t treat a diabetic as less than human, but we do treat people with addictions in this manner. It must change if we are to help the large portions of our population who come become addicted more effectively. But do we want to homogenize addictive drug and ignore the devastation that far too often comes with it? I hope not!
Destigmatizing drug users is far different than destigmatizing addictive drug use. There are taboos against addictive drugs for good reason, particularly in relation to addictive drug use by young people. We know that developing brains are more susceptible to addiction and that early drug use increases the risk of addiction. Most of us would not want to destigmatize heroin use for kids. Drug use is dangerous, we draw a fence around it and let people know it is dangerous for good reason. Look at what alcohol, a legal drug can do to a person and change their very nature as addiction takes hold. I don’t want my family members experimenting with methamphetamine. Cannabis related highway fatalities are dramatically increasing. I don’t want the driver in the car heading towards me to be impaired on cannabis or alcohol. We have to be able to talk about these very real and very tragic consequences. Open discourse about such things is becoming hard to do because of the dynamics of tribalism present in our community and in the larger society.
We do not want our babysitters high on heroin for good reason, but we should want to help the person and everyone so impacted. There are serious risks to public safety that come with drug use. We also know that people who use drugs heavily over time often experience significant changes to their personalities and do things they would not do in an era of life prior to their decent into addiction. We should feel compassion not derision.
We should not be chastising each other for talking about our own realities with severe addiction, even as there is growing awareness that there are people with less severe forms of substance use. Sugar coating the terrible consequences of severe addiction would be wrong of us, even as we work towards reducing stigma aimed at the persons who experience addiction and those of us in recovery to ensure fair treatment in society. Addiction is a deadly and serious condition, and we must acknowledge risks associated with addictive drug use even as we work to embrace our brothers and sisters in the grips of addiction.
While these are important conversations as a society and as a recovery community, we seem increasingly ill equipped to have them as we move away from nuanced open dialogue and into entrenched ideological camps in parallel with the rest of society. The latter dynamic is perhaps just as dangerous as destigmatizing addictive drug use, in my humble opinion. Many lives are in the balance and history shows us we can and do recover, and that once we do, we have the capacity to come together and do great things. Homogenizing what addiction looks like does not move us in that direction.