While you were actively using substances, you probably didn’t think much about your health. Substance use disorder shifts your motivation and attention to acquiring or actively drinking or using drugs. Let’s face it — no one wakes up after a day of using drugs or drinking feeling “great” or ready to run a marathon. These substances negatively impact your mental and physical well-being both during and long after usage has stopped. This is why during recovery, self-care is key to long-term success. Exercise is an excellent form of self-care that has infinite benefits.
Here are 5 ways exercise can help you be successful in your recovery:
Exercise can…..
-
Improve your sleep.
Getting the appropriate amount of sleep is a necessity for everyone, regardless of whether you are in recovery or not. It is not uncommon to experience difficulty sleeping if you once used substances to help you sleep. Sleep is restorative and a lack thereof can have profound consequences on the psyche. Lack of sleep not only makes us tired and sluggish during the day, less productive, and generally “moody”, but it also means we cannot fully appreciate the good that is around us, often obsessing over the negatives in our lives. Having enough sleep helps with our cognitive processes and allows us to make the best decisions as we continue the lifelong journey of recovery.
-
Improve your mood and confidence. (Acquiring endorphins, the healthy way!)
You know that flood of happiness you get from a piece of chocolate?As you exercise, your brain naturally releases Endorphins, Serotonin, and Dopamine, creating a feeling of improved life satisfaction and happiness.
-
Help to reduce stress.
Recovery is stressful. It requires daily dedication to staying well and staying sober. Life, in general, is stressful at times. Stress impacts our blood pressure, our hearts, our blood sugar, and more. In contrast to substances, exercise is an incredibly positive and healthy coping mechanism to combat the stressors you may face. Exercise is a stress buster and stress is a sobriety buster. Stress is a natural and normal part of everyday life, yet studies show it can be greatly reduced with consistent exercise. As you reduce your stress, you increase your mental capacity to face the challenges of day-to-day living.
-
Help you structure your days and set goals.
Set times throughout the week that you will be physical and stick to them as if they were a job! Build your schedule around these blocks and create a structure for your weeks. Finding structure, setting goals, and achieving them is one of the cornerstones of a successful recovery and long-term sobriety. We may measure our sobriety in days, months, or even years, but it is something that we cannot take for granted. The temptations of relapse are always present. In recovery, it is important to create interim, attainable goals with the ultimate goal of staying clean for the rest of our lives. Exercise promotes this healthy thinking as we see progress in our dedication, consistency, and physical abilities – how far we can run, how much weight we can lift, etc. Aligning our exercise goals with our recovery goals can make for a positive and self-fulfilling situation.
-
Help you connect and bond with others.
Exercise is a great way to bond with others and connect. Whether you find classes at your local gym or fitness groups online, physical activity provides yet another way to connect. Connecting with like-minded individuals, focused on self-care and health will only further strengthen your support network as you progress in your recovery.
Join us on July 9th at 7:00 PM EST for our recovery-based Mindfulness and Yoga Zoom session for Fellowship Hall Alumni. Check your email for the Zoom link and be sure to add it to your calendar! OR, email us to get the link.
AND
Join us on July 19th at 5:00 PM EST for our recovery-based Running Club in Greensboro for Fellowship Hall Alumni. Check your email for the meet-up location and more information and be sure to also add this to your calendar!
Ultimately the benefits of exercise are endless, and they speak for themselves. While it is only one part of the lifelong recovery process, it represents very real protection from drug use and relapse. And while many think that exercise needs to be difficult and take lots of time, exercise can be classified as anything that gets you moving, increases your heart rate, and makes you feel good. You should find ways to get active that you enjoy…make it FUN!
Here are some of our favorite workout videos, resources, and links:
Core Power Yoga
https://www.corepoweryogaondemand.com/
• Free access to yoga and meditation classes through Core Power on Demand.
Cross Fit at Home
https://www.crossfit.com/at-home/movements
• Provides free access to various workout and nutrition videos to preserve your health at home.
Daily Burn
https://dailyburn.com/landing#!home
• Sign up for a free 30-day trial and receive access to full body workouts daily, including cardio, yoga, dance, Pilates and more. • Credit card information required for the free trial.
Ekhart Yoga
https://relief.ekhartyoga.com/
• Offering 12 free yoga and meditation classes, specifically designed to help relieve stress and anxiety. TOGETHER WE ARE STRONGER!
Fitness Blender
https://www.fitnessblender.com/videos
• Offers free workout videos based on difficulty, focus, and equipment available.
Gold’s AMP
• Providing free access to over 600 audio and video workouts to keep you moving through May 2020. Use promo code FIT60
Nike Run Club
https://www.nike.com/nrc-app
• Need to get outside for a bit or have a treadmill at home? This free app helps you track your run and allows access to guided runs hosted by coaches or Headspace.
ObéFitness
https://www.obefitness.com/
• Live fitness classes with a 30-day free trial (use code ATHOME). • Will require credit card information for the free trial.
Peloton
https://www.onepeloton.com/app
• Their digital app is free for 90 days; you don’t need a Peloton to use it. Not only do they offer bike and treadmill classes, but they offer outdoor walking/running classes, strength, yoga and meditation.
Pop Sugar Fitness
https://www.youtube.com/user/popsugartvfit/about
• A free YouTube exercise channel that offers fitness tutorials and workouts.
10 Free Workout Apps to Use!
https://www.yahoo.com/lifestyle/free-workout-apps-social-distancing-coronavirus-184514493.html
Now get to moving! Share with us YOUR favorite ways to be active by tagging @FellowshipHallNC or using the hashtag #FellowshipNCFitness on Facebook or Instagram J
About Fellowship Hall
Fellowship Hall is a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.
I haven’t posted for some time.
The hospital I work at was hit very hard by COVID-19 and I’m still working on getting recharged for activities like blogging, but the pandemic did play a role in inspiring this post.
I’ve been thinking a lot about the convergence of several cultural trends:
- historically unprecedented access to information;
- the atomization of media and information sources;
- the tribalization of media and information sources;
- scientism as a cultural force that:
- lacks epistemic humility;
- is often dismissive of experiential knowledge;
- is often dismissive of outcomes that can’t be easily quantified and measured;
- faces a replication crisis;
- a crisis of faith in expertise and experts;
- an epistemic crisis creating a cultural inability to agree on facts (not the meaning of the facts, but the basic facts themselves);
- postmodern destabilization of traditional concepts and models, including addiction and recovery; and
- a cultural moral realignment from moral impulses like sanctity, authority, and loyalty to fairness and care.
How do these larger trends affect addiction, recovery, and treatment?
This is not an argument for or against anything, just a collection of observations as I’m trying to make sense of the pull and push forces affecting the field for better and for worse.
Information overload
20 years ago, getting information on heroin addiction would require speaking with a doctor or counselor, or visiting a library. Today, in 0.53 seconds, one can have access to more than 40 million web pages about heroin addiction.
Atomization of information
Access to information is a good thing, but how does one begin to approach 40 million units of information?

It’s unapproachable. And, if one of those pages is yours, how do you distinguish yourself and find an audience?
This sea of information is going to be segmented by author, audience, style, etc. Furthermore, this isn’t one unit of information repeated in 40 million places with differences in the way or place it’s presented. The internet and social media has made it possible for everyone to create content. This information itself varies widely in focus, depth, and accuracy.
This is what I’m referring to as atomization–one topic generating 40 million units of information and those units being spread and sorted across millions of information sources.
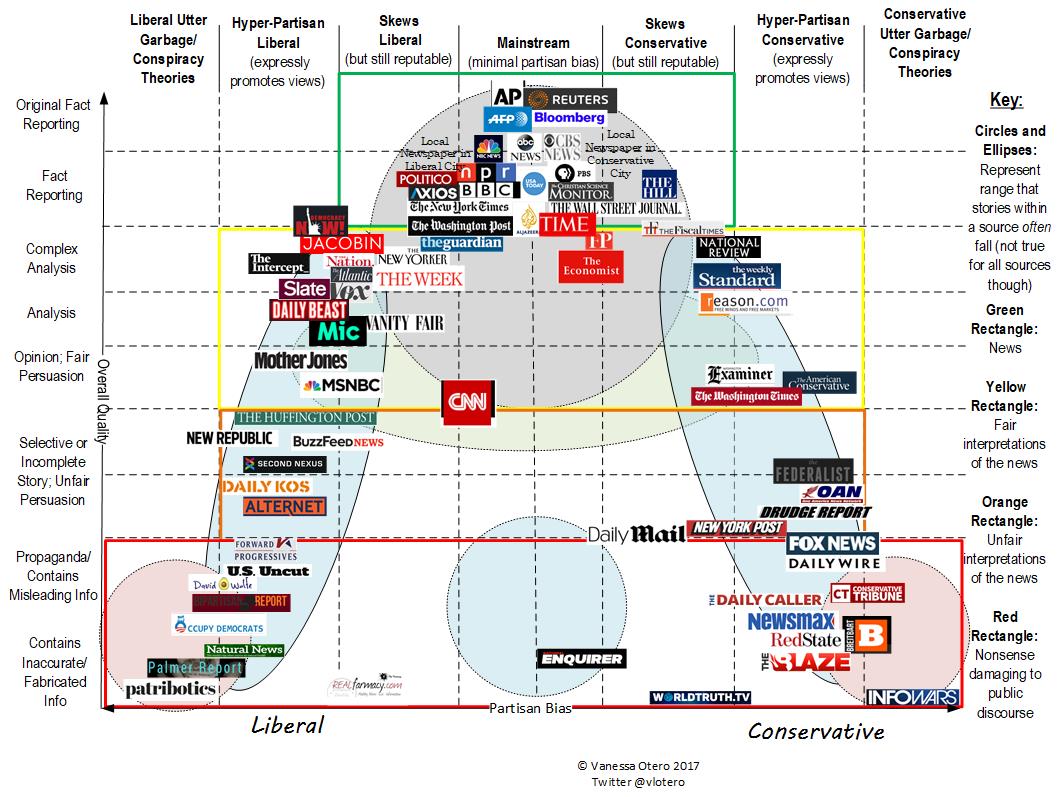
Tribalization of information
As information gets atomized, some of it might sort by audience–for example moms, kids, healthcare providers, etc. Other sorting will be focused on advancing one ideology or perspective, often at the expense of another.
This is where we get into medication vs. drug-free, 12 step vs. CBT, abstinence vs. harm reduction, medical vs. psychosocial, etc.
As information gets sorted by these tribes, actors create their own content for their own tribe. Information sources become trusted not because of their rigor and accuracy but because of their fidelity to the messages/goals/values of the tribe. This elevation of fidelity to the cause over truth results in echo chambers and feedback loops that are increasingly unmoored from truth and isolated from conflicting information. These echo chambers increase tribalization by elevating the most extreme voices and escalating tension with other tribes through misinformation, straw men, and attribution of bad motives.
Scientism
While there’s no single definition of scientism, it generally refers to “the idea that all forms of intellectual inquiry must conform to the model(s) of science in order to be rational.” The term is often used pejoratively when science is invoked to dismiss an argument or position.
The premise that science can answer all questions sets up a few conflicts.
- If science can answer all questions, science can tell us what to value. Values that are not rooted in science can only lead us astray. They have no place in decisions about policies or treatments for addiction.
- Science values what can be measured and tested. It favors outcomes that can be easily quantified and measured. Abstract outcomes like “better than well” and outcomes that take years to evaluate are dismissed by scientism.
- Science-based arguments can often be constructed to support more than one position, including conflicting positions.
- Invocations of science often (knowingly or unknowingly) conceal values behind policy or treatment positions.
- Experiential knowledge is dismissed as anecdotal and invalid.
Moreover, medicine and the social sciences are facing a replication crisis that is unacknowledged by many advocates and used by others as a reason to dismiss scientific knowledge all together. One would hope that this would lead to epistemic humility, but seems like too great a hope.
A crisis of faith in experts
I recently heard a few relevant observations:
- Too many people think expertise means having a lot of information about something. And, as noted above, people have unprecedented access to information today. Having information does not make one an expert. Expertise is information plus experience.
- Experts (and politicians) are expected to have answers to questions that no one has answers for. We punish them for not knowing and then seek people who will provide an answer.
- Martin Gurri noted the following about COVID-19, “The experts, the people who knew the most, didn’t know that much, but they had to pretend that they did. And, that’s where you get in trouble.”
Epistemic crisis
This crisis of faith in experts (and the other trends) creates the conditions for an epistemic crisis, which David Roberts described as a split “in who we trust, how we come to know things, and what we believe we know — what we believe exists, is true, has happened and is happening.”
Similarly, Martin Gurri described the 21st century as post-truth, “as I define it, signifies a moment of sharply divergent perspectives on every subject or event, without a trusted authority in the room to settle the matter.”
This is a larger cultural phenomenon with disputes about whether there are caravans of foreigners entering the country, whether voter fraud is a widespread problem, and whether COVID-19 is under control.
In our space we see arguments about whether 12 step programs are effective, whether MAT is effective, the dangers of various drugs, whether one can OD on fentanyl by touching it, whether opioid prescribing had anything to do with the opioid crisis, whether moderate use is an appropriate goal for people with addiction, etc.
The explosion of information has eroded deference to experts by providing a platform for dissident experts, and exposing intentional and unintentional misinformation from experts. The internet and social media has also provided a platform for anyone to claim expertise. Expert status used to be a result spending time in institutions learning and practicing. These institutions were formative–they molded people. The new information landscape allows people to claim expertise outside of these institutions. It also allows people who have not yet been molded by an institution to use an association with the institutions to promote themselves.
It’s worth noting that our field has its own history of experts overstating the harms of many drugs, the prevalence of some drugs, over-extending the concept of addiction, and over-diagnosing addiction (particularly in young patients).
Destabilization of shared concepts
All of the above create the conditions for not just instability in our ability to determine or agree upon what’s true, but whether our underlying assumptions are true. Whether things like addiction and recovery are just social constructs.
For example, recent years have witnessed questions about:
- Whether addiction is a valid concept, or whether it’s chaotic use related to trauma and/or environmental conditions.
- Whether addiction is a prerequisite for recovery.
- Whether most of the harms associated with “addictive” drug use are due to it’s social and legal status.
- Whether “recovery” can include use of alcohol, tobacco, or non-prescribed use of substances with addiction potential.
- Whether definitions of recovery even need to address alcohol and other drug use.
Moral realignment
Realignment might be too strong a word here, but let me explain what I’m thinking.
Jonathan Haidt’s moral foundations theory suggests that there are 5 (or 6) universal moral impulses underlying the moral systems of every culture. The 5 (and the proposed 6th) moral impulses are:
- Care/harm
- Fairness/cheating
- Loyalty/betrayal
- Authority/subversion
- Sanctity/degradation
- Liberty/oppression
They believe everyone values each impulse to some degree but values some more than others. (It’s worth noting that a moral impulse can be expressed in a broad range of ways. For example, sanctity may be expressed as sexual purity or as eating “clean.”)
They’ve also proposed that political ideology predicts the moral judgments. Liberals tend to emphasize the Care, Fairness and Liberty dimensions (characterized as individualizing); conservatives the Loyalty, Authority and Sanctity dimensions (characterized as binding).
While political power is unstable and shifting frequently, it could be argued that liberals are winning the culture and that this is resulting in a increasing cultural emphasis on care, fairness and liberty while diminishing loyalty, authority and sanctity.
This invites the question, how does this affect beliefs about drug use, addiction, recovery, and drug policy?
Follow the science!
One of the things that brought this post to mind watching the coverage of the COVID-19 pandemic unfold. It seemed like an opportunity to restore faith in experts and institutions. Unfortunately, we watched a lot of these patterns repeat themselves.
One of the refrains I heard frequently was “follow the science!”
I hear this a lot in addiction treatment and recovery too. I find it frustrating. Not because I don’t value science, but I find that a useless statement.
My response is, “follow the science to what?”
Science can help us understand what is and what is possible, but it can’t tell us what endpoint to want. And, the trends above will shape our understanding of the problem(s), the solution(s), the good, etc.
For example, with COVID-19, the question may be, “what course of action would result in the fewest deaths and is medically, socially and economically sustainable for up to 18 months?” In the case of addiction treatment, the question may be which treatment will “get me back to the way I used to be” or “help me have a normal life with a job, a house, kids, friends and family.”
Science can provide valuable data and clues to help us achieve our goals, but it can’t answer many of the questions that are most important to us.
Unfortunately, conversations about these questions and the trends that shape the discussion do not lend themselves to social media posts.
Event Description
The North Carolina Department of Health and Human Services (NCDHHS) is pleased to announce the first Olmstead Plan Stakeholder Advisory (OPSA) quarterly, online meeting. The U.S. Supreme Court's ruling in Olmstead v. L.C. set the bar for accelerated community inclusion and reduced reliance on institutional care for people with disabilities, across a life span. Since that ruling, our system has been steadily evolving. Now, it is time to take it to the next level with a plan that will advance innovation, coordination and whole-person, systemic change. The Office of the Senior Advisor for the Americans with Disabilities Act (ADA) and Olmstead will lead this 18-month initiative. OPSA's first quarterly, online meeting to be held on July 8 from 2:00 PM to 5:00 PM.
The OPSA will be diverse, inclusive of people with lived experience, family members, advocacy groups, policymakers, regional management entities, providers, members of the General Assembly, and others. The Boston-based Technical Assistance Collaborative (TAC) will provide technical support, along with professionals from across NCDHHS. With Olmstead-based work already taking place in NCDHHS, our foundation for continued progress is strong. With the help of OPSA, we will develop a roadmap that is data-driven, outcome-based, person-centered and aligned to realize Olmstead's promise of welcoming and supportive communities.
Please join us if you’d like to participate in the first open discussion as we collaborate with a diverse group of individuals to assist in the development of the Olmstead Plan.
Sign language interpreters will be available.
When:
Wednesday, July 8, 2020 - 2:00 pm to 5:00 pm
Where:
Join Zoom Meeting: https://zoom.us/j/91963131476?pwd=UTN3akpGT2phUWJOVkVrVzk3VEJSZz09
Meeting ID: 919 6313 1476
Password: 811590
Marijuana Concentrates DrugFacts
amartinek
Thu, 06/25/2020 - 13:06
Cannabis plants are covered by microscopic, mushroom-shaped, hair-like compounds called trichomes. These outgrowths surround the budding marijuana flower and produce the plant’s cannabinoids. Different varieties of trichomes can be collected. The resulting products—collectively called cannabis concentrates—can contain very high levels of tetrahydrocannabinol, commonly referred to as THC, the psychotropic ingredient in marijuana. These THC-rich marijuana products may be vaporized and inhaled using a vape pen or through a process called dabbing.1
How are concentrates made?
Marijuana concentrates can be made in a commercial environment with modern equipment or prepared in a home setting.2 They are produced in various ways, including:
- dry processing (kief, finger hash)
- dry ice processing
- water-based processing (bubble hash)
- combining pressure with heat
- using nonflammable carbon dioxide solvents
- using flammable solvents, including butane (lighter fluid), propane, ether or alcohol1
Using flammable solvents is popular because the products have high THC levels,1 users report longer-lasting effects,1 and it is a relatively inexpensive and efficient production method.2 Butane is a commonly used solvent, producing the potent marijuana concentrate butane hash oil (BHO), also known as amber, dab, glass, honey, shatter, or wax.2
What does the final product look like?
The products resulting from these methods may be:
- a gooey liquid wax (hash oil or honey oil)
- a soft solid with a texture like lip balm (wax or budder)
- a hard, amber-colored solid (shatter)
Hash oil and waxes can be consumed using vape pens. Solids can also be placed on a heated platform usually made of titanium, quartz, or ceramic, where they are vaporized by high heat and inhaled through a dabbing tool, often called a rig.2
What’s the difference between concentrates, extracts, and dabs?
The terms used to describe these products vary. Concentrates is a broad term referring to all products that have been extracted from the plant. Although extracts and concentrates are often used interchangeably, some people define extracts as products manufactured using solvents, but not those pulled from the plant with non-solvent methods. Dabs may refer to products made exclusively from butane hash oil; however, the term is sometimes used colloquially for concentrates extracted in other ways. There are also post-production methods that lead to further variations in products and terms.3
What are the health effects of concentrates?
There are adverse effects associated with marijuana use in any form,3 though additional research is needed to understand how the use of concentrate may differ from smoking dried marijuana buds. Marijuana concentrates have very high levels of THC. Solvent-based products tend to be especially potent, with THC levels documented at an average of about 54-69% and reported to exceed 80%, while non-solvent based extraction methods produce average THC levels between 39-60%.4 In comparison, the THC content in marijuana plant material, which is often used in marijuana cigarettes, is lower—with samples seized by the U.S. Drug Enforcement Agency averaging just over 15%.5 Not only do concentrates have high levels of THC, but dabbers inhale the entire amount all at once—in a single breath.2 As a result, concentrates can deliver extremely large amounts of THC to the body quickly. The risks of physical dependence and addiction increase with exposure to high concentrations of THC, and higher doses of THC are more likely to produce anxiety, agitation, paranoia, and psychosis.6 Additional research is needed to understand how the use of concentrate affects these risks.
In addition, contaminants in concentrate products may be cause for concern. One study noted that 80% of tested concentrate samples were contaminated in some form, not only with pesticides (which is also a concern for dried bud), but also with residual solvents that were not fully purged in the manufacturing process. Users of BHO, for example, likely inhale some butane and other impurities along with the vaporized THC.2 It is important to note that direct inhalation of concentrated butane among recreational inhalant users carries multiple risks, including reported deaths.7 However, it is unclear what negative health outcomes result from the inhalation of residual butane, other solvents, or leftover contaminants during the dabbing process.
Is it dangerous to make solvent-based concentrates?
When solvents are used to produce concentrates, the preparation process itself can be dangerous. A number of people using butane to make extracts at home have caused fires and explosions and have been seriously burned.8 A study conducted in 2015 looking at implications from marijuana legalization in Colorado reported that in a 2-year period the University of Colorado burn center saw a substantial increase in the number of flash burns that occurred during amateur THC extraction using butane, some involving more than 70% of body surface area and most requiring skin grafting.9
It is against federal law to manufacture BHO,10 and even in some states where adult use of marijuana is legal, like Colorado and California, it is illegal to make hash oil using flammable liquids. In Colorado, state officials recommend alternate methods using nonflammable dry ice (CO2), ice water, or purchasing the product from a licensed marijuana retail store.11 Most licensed, commercial production facilities use a safer extraction system that prevents solvents from being wasted or exposed to the open air where they could inadvertently be ignited, similar to decades-old systems used in the production of many commercial products.2
Points to Remember
- Cannabis plants are covered by microscopic, mushroom-shaped, hair-like compounds called trichomes which surround the budding marijuana flower and produce the plant’s cannabinoids.
- Trichomes can be collected and made into concentrates, including extracts and dabs.
- Concentrates can contain very high levels of THC, the psychotropic ingredient in marijuana.
- Concentrates can be vaporized and inhaled using a vape pen or by dabbing.
- Concentrates can be made in commercial settings or in a home through several methods, including dry ice- and water-based processing and the use of solvents.
- Using flammable solvents, such as butane, propane, ether or alcohol, is popular because it produces high THC levels, longer-lasting effects, and it’s relatively inexpensive.
- Using butane as a solvent produces the potent marijuana concentrate butane hash oil (BHO), also known as amber, dab, glass, honey, shatter, or wax.
- Exposure to high levels of THC increases the risks of physical dependence and addiction. Higher doses of THC are more likely to produce anxiety, agitation, paranoia, and psychosis.
- Contamination with pesticides and residual solvents that weren’t fully removed during production is a concern. People who use BHO likely inhale some butane and other impurities along with the vaporized THC.
Learn More
For more information about marijuana and marijuana use visit
References
- Raber JC, Elzinga S, Kaplan C. Understanding dabs: Contamination concerns of cannabis concentrates and cannabinoid transfer during the act of dabbing. J Toxicol Sci. 2015;40(6):797-803. doi: 10.2131/jts.40.797
- Al-Zouabi I, Stogner JM, Miller BL, Lane ES. Butane hash oil and dabbing: Insights into use, amateur production techniques, and potential harm mitigation. Subst Abuse Rehabil. 2018;9: 91–101.
- Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse Health Effects of Marijuana Use. N Engl J Med. 2014;370(23): 2219–2227. doi:10.1056/NEJMra1402309.
- Meier MH, Docherty M, Leischow SJ, Grimm KJ, Pardini D. Cannabis concentrates use in adolescents. Pediatrics. 2019;144(3):e20190338. doi:10.1542/peds.2019-0338.
- National Institute on Drug Abuse. Is marijuana addictive? drugabuse.gov. https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-addictive. Updated April 8, 2020. Accessed June 17, 2020.
- Freeman TP, Winstock AR. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45(15):3181-9. doi: 10.1017/S0033291715001178.
- Sironi L, Amadasi A, Zoja R. Recreational inhalation of butane and propane in adolescents: Two forensic cases of accidental death. Forensic Sci Int. 2016;266:e52-e58. doi: 10.1016/j.forsciint.2016.05.028.
- Romanowski KS, Barsun A, Kwan P, et al. Butane hash oil burns: A 7-Year perspective on a growing problem. J Burn Care Res. 2017;38(1):e165-e171. doi: 10.1097/BCR.0000000000000334
- Monte AA, Zane RD, Heard KJ. The implications of marijuana legalization in Colorado. JAMA. 2015;313(3):241-2. doi: 10.1001/jama.2014.17057.
- Two charged in connection with drug lab explosion. dea.gov. https://www.dea.gov/press-releases/2018/09/06/two-charged-connection-drug-lab-explosion. Published September 6, 2018. Accessed June 17, 2020.
- Safety with hash oil. Colorado.gov. https://www.colorado.gov/pacific/marijuana/safety-hash-oil. Accessed June 17, 2020.
This publication is available for your use and may be reproduced in its entirety without permission from NIDA. Citation of the source is appreciated, using the following language: Source: National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.
Office of Research Training, Diversity, and Disparities (ORTDD)
What We Do
The Office of Research Training, Diversity, and Disparities (ORTDD) offers a wide range of programs, workshops, and funding mechanisms to support the development of substance use and addiction research scientists throughout the career pipeline. The ORTDD is committed to providing training opportunities to ensure a cutting-edge diverse research workforce that will advance the knowledge base needed to address urgent public health substance use and addiction problems.
Offices within the ORTDD
The Office of Research Training and Career Development (ORT)
The Office of Research Training and Career Development (ORT) provides research grants to promising scientists to meet the Nation’s need for drug abuse and addiction research. NIDA’s portfolio includes research in basic, clinical, and translational sciences. Read more about the NIDA ORT career development fellowships and grants.
Introduction to Research Training at NIDA
NIDA offers a strategic set of funding mechanisms to support the development of research scientists through multiple stages of their careers. These awards are designed to ensure that scientists of the very highest caliber are available to meet the Nation’s need for substance use and addiction research. NIDA’s portfolio includes research in basic, clinical, and translational sciences. This includes genetics, epigenetics, molecular biology, neuroimaging, cognitive and social neuroscience, pharmacological and behavioral therapies, prevention, epidemiology, health services, health disparities, HIV/AIDS and other related domains. NIDA also promotes opportunities for quantitative scientists from fields such as mathematics, bioengineering, and physics to apply their knowledge to the study of substance use and addiction.
The Office of Diversity and Health Disparities (ODHD)
The Office of Diversity and Health Disparities (ODHD) offers programs to help undergraduate and graduate students, postdoctoral fellows, and early-stage investigators from underrepresented backgrounds launch their independent research careers. NIDA aims to enhance the representation of these scientists in the biomedical research workforce through outreach, education, and other research training initiatives. Read more information about NIDA ODHD programs and initiatives.
What We Do
To enhance the pool of underrepresented populations in the sciences, the National Institute on Drug Abuse established the Office of Diversity and Health Disparities (ODHD) 20 years ago. The mission of the ODHD is to strengthen the NIDA extramural research portfolio through a more diverse and robust extramural research workforce, attracting and retaining talented individuals from all populations in order to fulfill the mission of NIDA. The ODHD’s goals are to:
- Promote and support underrepresented scholars and researchers actively participating in research;
- Enhance the pool of underrepresented scholars and researchers independently funded to conduct substance abuse research;
Ensure that research addressing health disparities is adequately represented in NIDA’-supported substance abuse research.
Underrepresented researchers face a number of challenges that influence their success in obtaining independent support from NIDA, the NIH, and other federal funding agencies. Some of these challenges include limited/poor mentoring, lack of adequate knowledge of NIH funding opportunities and processes, limited access to novel high priority research projects and design, low publication records, and limited professional networking to successfully bridge to the next career level. Collectively, these factors impact NIDA's efforts to retain underrepresented investigators conducting substance abuse research and further develop the research infrastructure within this community. To that end, NIDA has implemented several key early stage outreach programs which play a vital role at recruiting, training, and retaining underrepresented researchers from underrepresented backgrounds in order to develop and support their research careers.
area
Wed, 06/24/2020 - 12:04
 Charles True has been building the kind of life he doesn’t want to relapse from for many years. His project work has taken him around the world including China, Russia, and the United Kingdom. One of his most impactful projects is the InsideOut® program. InsideOut is a cognitive-based therapy (CBT) program for substance abuse treatment […]
Charles True has been building the kind of life he doesn’t want to relapse from for many years. His project work has taken him around the world including China, Russia, and the United Kingdom. One of his most impactful projects is the InsideOut® program. InsideOut is a cognitive-based therapy (CBT) program for substance abuse treatment […]
 We are pleased to announce the release of our newest Tips & Tools for Recovery that Works! video Let’s Talk About Urges. In this video we define urges, identify misconceptions about urges, and offer tools for coping with urges. Checkout the SMART Toolbox for additional resources. Click here to watch this helpful video on our YouTube channel. Subscribe to […]
We are pleased to announce the release of our newest Tips & Tools for Recovery that Works! video Let’s Talk About Urges. In this video we define urges, identify misconceptions about urges, and offer tools for coping with urges. Checkout the SMART Toolbox for additional resources. Click here to watch this helpful video on our YouTube channel. Subscribe to […]
 David Weidman is fond of a quote by past SMART Recovery president Dr. Tom Horvath: “There are as many paths to recovery as there are people trying to recover.” For Weidman, a nontheist who wanted to conquer his OxyContin addiction on his own terms, the path to recovery led directly to SMART. “I read that […]
David Weidman is fond of a quote by past SMART Recovery president Dr. Tom Horvath: “There are as many paths to recovery as there are people trying to recover.” For Weidman, a nontheist who wanted to conquer his OxyContin addiction on his own terms, the path to recovery led directly to SMART. “I read that […]
 Provided by SMART Family & Friends Facilitator, Kerry Hammell In the fall of 2018, I started the SMART Recovery Family & Friends meeting in Campbell River on Vancouver Island, B.C., Canada. It quickly developed a regular following of 10-15 participants that often reported that the meetings were providing each of them with tremendous support and encouragement. Then came COVID-19 in March […]
Provided by SMART Family & Friends Facilitator, Kerry Hammell In the fall of 2018, I started the SMART Recovery Family & Friends meeting in Campbell River on Vancouver Island, B.C., Canada. It quickly developed a regular following of 10-15 participants that often reported that the meetings were providing each of them with tremendous support and encouragement. Then came COVID-19 in March […]
NIDA Researchers Adapt Their Projects to Study COVID-19
mfleming
Mon, 06/15/2020 - 21:54
The U.S. is now facing two intersecting health crises, the ongoing opioid overdose epidemic and the COVID-19 pandemic. Regrettably, each has the potential to exacerbate the effects of the other. In March, NIDA released a Notice of Special Interest to alert researchers with existing grants to our interest in supporting applications for administrative supplements and urgent competitive revisions that could be used to investigate aspects of COVID-19 as they intersect with substance use and related areas in NIDA’s research portfolio, like HIV. These applications are being reviewed on a rolling timeline (and we will continue to update this blog as new supplements are awarded).
NIDA has thus far issued nearly $4 million in funding for COVID-19-related projects that could leverage current infrastructure, projects, or scientific knowledge and resources. Those projects range from assessing the virus’s impact on individuals with a substance use disorder (SUD), including those who are homeless or incarcerated, to basic research to investigate potential interactions between drugs and COVID-19, including effects on the immune system. At the same time, researchers at NIDA’s Intramural Research Program (IRP) quickly responded to the pandemic with new ideas to exploit their knowledge and research capabilities.
Since substance use may put people at increased risk for infection with SARS-CoV-2 or the most serious outcomes of COVID-19, several research projects will be assessing this. Smoking and vaping—both of nicotine and cannabis—may be risk factors for worse COVID-19 outcomes, so we are funding supplements to examine COVID-19 in people who smoke and/or vape. A project at Boston University will use single-cell transcriptomics (a method to study gene expression via RNA) to examine whether smoking and vaping are risk factors for severe COVID-19 and its associated cytokine storm—an immune response that proves fatal in some patients. Researchers at the University of Tennessee-Knoxville studying the effects of text-messaging-delivered peer network counseling in young adults with cannabis use disorder will use supplemental funding to examine the impact of COVID-19 on health, smoking/vaping, and other substance use behaviors in this population.
The NIDA-funded National Drug Early Warning System (NDEWS) is a network of researchers at 18 sites across the country collecting and sharing data on drug use trends. With new supplemental funds, NDEWS will be expanding its efforts to track substance-use-related COVID-19 consequences in several urban, rural, and suburban areas with the help of local informants including funeral directors, emergency medical technicians, and staff at syringe services programs, to rapidly share the information gathered.
NIDA-funded researchers at the University of California-San Diego are looking at social networks, drug markets, and drug tourism among people who inject drugs in San Diego and Tijuana. Supplemental funds will enable them to expand their study to test this population for SARS-CoV-2 infection using nasal and fecal samples. This data will provide information about transmission of the virus among people who use drugs on both sides of the US-Mexico border and potentially inform policymakers about the impact of proposed mitigation strategies such as closure of the border.
Social distancing to prevent the spread of the coronavirus may lead to more individuals using drugs alone, raising the risk of overdose because bystanders may not be present to intervene or may be reluctant to intervene. Another project by researchers at New York University will study the effects of COVID-19 on opioid overdose risk behavior and how it is affecting access to and use of naloxone. The need for social distancing has increased the use of telemedicine and has resulted in the relaxation of rules governing the dispensing of controlled medications like methadone and buprenorphine. Building on their ongoing study of HIV/hepatitis and opioid prevention and treatment, supplemental funds will allow researchers at Oregon Health and Science University to examine how opioid treatment programs are implementing the new policy allowing four weeks’ worth of take-home doses of methadone for stable patients (and two weeks’ worth for others, based on clinics’ discretion), as well as assess the effects of this change. The researchers will also analyze Medicaid claims to study COVID-19 diagnoses and estimate treatment burden among people with opioid use disorder.
Social distancing has also made it harder to access behavioral treatment and recovery supports.
NIDA research has already supported numerous devices and apps to help people with SUD connect virtually to peers and counselors, and some startups are adapting their innovations to address the COVID-19 crisis. Researchers at the University of Wisconsin-Madison are using a NIDA supplement to adapt their ACHESS smartphone recovery app to help users with social distancing, adjusting to isolation, and using virtual SUD treatment and recovery services. They will also assess the impact of their app on users’ anxiety, loneliness, and reported COVID-19 infections.
An ongoing study by NIDA IRP researchers finding ways to measure psychosocial stress in people receiving treatment for OUD is being modified to allow participants to complete questionnaires and answer questions online rather than visiting a clinic or physically engaging with research staff. This will enable the researchers to measure the impact of COVID-19 on recovery, relapse, and medication adherence in this group.
Several projects are also looking at COVID-19 as it relates to HIV. Using supplemental funds to their existing grant to study implementation of pre-exposure prophylaxis for HIV prevention (PrEP) among people who inject drugs, researchers at Boston University Medical Campus will interview clients and staff of syringe-service programs to assess the impact of COVID-19 on drug markets, HIV-risk behaviors, use of HIV prevention services, and the way those services have adapted to the pandemic.
Two projects, one at the University of Maryland, Baltimore, and another at Massachusetts General Hospital, will also examine how underlying HIV infection affects COVID-19 disease progression in people who use opioids. A project at Johns Hopkins University will study barriers to receiving drug treatment and HIV/HCV care caused by the requirements of social distancing during the COVID-19 pandemic. And a study by researchers at the University of Miami School of Medicine will examine whether there are synergistic associations of methamphetamine use and HIV with SARS-CoV-2 prevalence in men who have sex with men.
Another especially vulnerable population is mothers and their children, in part because of limited access to health services during the pandemic. Researchers at Oklahoma State University for Health Sciences who are doing a feasibility study related to the proposed HEALthy Brain and Child Development (HBCD) study will use supplemental funds to assess the ability of pregnant women and new mothers (both with and without a history of SUD) to access treatment and mental health services during the COVID-19 crisis. Researchers at seven other sites across the country who are already recruiting pregnant and postpartum women for the HBCD study will also examine COVID-19’s impact on birth outcomes, parenting stress, and early childhood developmental milestones.
Researchers in the ABCD Study, now in its third year of data collection, will also leverage their infrastructure by surveying participating children and their parents about the impact of COVID-19 and the associated social, behavioral, and economic impacts on multiple aspects of their lives. A subset of children (N=500) who were issued Fitbits prior to the COVID-19 shutdown of schools and research site visits, continue to wear their devices so that information about their physical activity and sleep before, during, and after pandemic can be studied and compared.
Basic research supported by NIDA could also contribute to the development of new treatments for COVID-19. The Coronavirus-2 spike protein is known to bind to human angiotensin converting enzyme 2 (ACE2) receptors, and this is the focus of multiple investigations. A two-year project by researchers at Icahn School of Medicine at Mount Sinai will seek to identify molecules that could block this interaction, keeping the virus from invading host cells; they will also screen potential COVID-19 medications for interactions with medications used to treat SUD. A lab at NIDA’s IRP in Baltimore will also study the SARS-CoV-2 spike protein’s binding and affinity for various human cell types and test possible molecules that could be therapeutically useful.
A team at Scripps-Howard Research Institute has already developed a type of therapeutic agent (aminoadamantane nitrates) that has a protective effect on the neurons of people with Alzheimer’s disease and of people with HIV who use methamphetamine. These agents show activity in the ion channel in the envelope of the SARS-CoV-2 virus and may be able to enter it, so these compounds will be tested as possible molecular “warheads” to disrupt viral activity. Since viruses can cause damaging stress responses in a cellular structure called the endoplasmic reticulum, another laboratory at the NIDA IRP will test the effects of FDA-approved and novel drugs that might modulate these responses in the context of SARS-CoV-2 infection.
Pandemics are devastating, and COVID-19 is proving to be no exception, coming while America is already in the midst of the opioid crisis. But we now live in a world where science can be quickly mobilized to find solutions to mitigate its worst effects. Along with the other Institutes and Centers of the NIH, NIDA has swiftly responded to the COVID-19 crisis by supporting research in areas of basic science, prevention, treatment, epidemiology, and implementation, particularly at the intersection with SUD. I am hopeful that these supplemental funds will contribute to lessening the impact of the collision between the opioid and COVID-19 crises.





Add new comment