Association between cell density at baseline (measured by restriction spectrum imaging) and change in waist circumference one year later. Cellularity in the ventral striatum demonstrates the strongest relationship among all regions in the subcortex
Differences in the microstructure of the nucleus accumbens (NAcc), a region in the brain that plays an important role in processing food and other reward stimuli, predict increases in indicators of obesity in children, according to a study funded by the National Institute on Drug Abuse (NIDA) and nine other institutes, all part of the National Institutes of Health. The paper, published today in the journal Proceedings of the National Academy of Sciences, is based on data from the Adolescent Brain Cognitive Development (ABCD)SM Study. The ABCD Study® will follow nearly 12,000 children through early adulthood to assess factors that influence individual brain development and other health outcomes.
Findings from this study provide the first evidence of microstructural brain differences that are linked to waist circumference and body mass index (BMI) in children. These microstructural differences in cell density could be indicative of inflammatory processes triggered by a diet rich in high fat foods.
“We know that childhood obesity is a key predictor of adult obesity and other poor health outcomes later in life,” said Nora D. Volkow, M.D., director of NIDA. “These results extend previous animal studies to reveal what may prove to be a vicious cycle in which diet-related inflammation in brain striatal regions promotes further unhealthy eating behaviors and weight gain.”
Evidence from past human imaging studies has demonstrated the relationship between the NAcc and unhealthy eating behavior in adults. In this study, the researchers leveraged new diffusion MRI imaging techniques to examine the cellular structure of areas that comprise the striatal reward pathway in the brain to investigate disproportionate weight gain in youth.
This study included data from 5,366 ABCD Study participants, ages 9- to 10-years-old at baseline, of whom 2,133 returned for a one-year follow-up visit. The mean waist circumference of the participants, used here as a measure of body fat, increased an average of 2.76 centimeters per participant from the baseline through the one-year follow-up. The researchers used a noninvasive MRI technique to show that an alleged marker of cellular density in the NAcc reflected differences in waist circumference at baseline and predicted increased waist circumference at one-year follow-up.
Because the ABCD Study is longitudinal, it will allow to assess if this association holds or changes over the course of adolescent development, and what factors may influence this trajectory.
Obesity in the United States affects approximately 35% of children and adolescents and is associated with negative health consequences, mentally and physically, as well as higher mortality rates. Children who are obese have more than a fivefold likelihood of becoming obese as adults. Predictive models of weight gain in youth, coupled with knowledge about factors that could impact this trajectory, would benefit public health and individual wellbeing.
Reference:
Rapuano, KM; Laurent, JS; Hagler, Jr. DJ; Hatton, SN; Thompson, WK; Jernigan, TL; Dale, AM; Casey, BJ; Watts, R. Nucleus accumbens cytoarchitecture predicts weight gain in children. PNAS. October 12, 2020.
September is Recovery Month, an occasion to focus on the needs of the millions of people in the U.S. living with a substance use disorder (SUD) as well as celebrate those who are trying or succeeding in putting drug use behind them. The stress and isolation of the COVID-19 pandemic are presenting enormous challenges for these individuals, but ultimately the altered realities of healthcare may create opportunities to reach more people with services and possibly even increase the reach of recovery support systems.
Significant increases in many kinds of drug use have been recorded since March, when a national emergency was declared and our lives radically changed due to lockdown and the closure of businesses and schools. In late April/early May, the Addiction Policy Forum (APF) conducted a survey of 1,079 people with SUDs nationwide, on how they were being impacted by the pandemic. Twenty percent of the respondents reported that their own or a family member’s substance use had increased since the start of the pandemic. And an analysis of a nationwide sample of 500,000 urine drug test results conducted by Millennium Health also showed steep increases following mid-March for cocaine (up 10 percent), heroin (up 13 percent), methamphetamine (up 20 percent) and non-prescribed fentanyl (up 32 percent).
Comprehensive national data are not yet available on overdoses, but data from some states such as Kentucky and Georgia as well as anecdotal reports suggest increases in overdose deaths and drug-related emergency room admissions in the first half of 2020 compared to last year. The Overdose Detection Mapping Application Program, a surveillance tool developed by the Washington/Baltimore High Intensity Drug Trafficking Area (HIDTA), reported increases in overdose reports in 62 percent of participating counties nationwide, and that overall overdose report submissions increased by 18 percent after stay-at-home orders commenced in mid-March. Clusters of overdoses seemed to shift from urban centers to suburban and rural locations. (One state, Kentucky, subsequently experienced a decline in overdoses after the state reopened.) In the APF survey, 4 percent of respondents reported an overdose since the beginning of the pandemic.
There are many anecdotal reports that people with SUDs are having to wait longer to obtain treatment, and closures of treatment centers have also limited access. More than a third (34%) of the respondents in the survey by APF had experienced disruptions accessing treatment or recovery support since the start of the pandemic, and 14 percent said they were unable to obtain needed services. There are reasons to expect that lower-income people and minorities could be especially affected. Despite implementing widespread COVID-19 testing, community health centers, which predominantly serve disadvantaged populations, are seeing declines in patient visits and are experiencing staffing problems.
The good news is that policy changes facilitating telehealth and expanding access to medications for opioid use disorder may compensate somewhat for these problems. People with opioid use disorders can now begin treatment with buprenorphine without an initial in-person doctor visit, which used to be the rule. Methadone treatment previously required daily supervised dosing with tightly controlled take-home options, but patients deemed stable may now obtain 28 days of take-home doses; others may receive 14 days of doses. Changes to Medicare and Medicaid rules are also enabling telemedicine consultations for SUD to be reimbursed more easily. These developments may particularly benefit people who live in rural areas or who otherwise have had trouble accessing treatment in the past, and NIDA has provided supplemental funds to grantees to evaluate the impact of such changes. Inevitably, since many people with SUDs do not have computers or smartphones, other innovative methods, such as combining telemedicine with street outreach, will be critical to ensuring that all people receive the care they need.
The stresses of the pandemic and the social isolation resulting from distancing measures may take an especially great toll on people trying to achieve or in recovery from an SUD. Three quarters of the APF survey respondents reported emotional changes since the beginning of the pandemic, especially increased worry (62%), sadness (51%), fear (51%), and loneliness (42%). These emotions increase the risk for relapse, and unfortunately, circumstances since the pandemic have made peer support, for instance in 12-step meetings and similar groups, much more difficult.
While online recovery supports may not be an option for all and cannot fully capture the in-person experience, here, as in the realm of treatment, teleconferencing tools and smartphone apps are helping some people adapt to restrictions on physical gatherings. Several of the startups NIDA has helped through our Office of Translational initiatives and Program Innovations, for instance, have now adapted their tools to deliver counseling or facilitate peer connection during COVID-19.
COVID-19 continues to be an uncertain, ever-evolving reality, and its impacts are particularly being felt among those with addiction and those in recovery from substance use disorders. At this point, there is very sparse data on how SUDs are affecting COVID-19 susceptibility and outcomes, although findings are emerging and I will address them in a future blog. As we think about and support this community, this month and every month, we need to imagine and implement new ways of facilitating treatment delivery and needed recovery supports under these new circumstances.
Research at the Intersection of HIV with Substance Use Disorders amidst the COVID-19 Pandemic
mfleming
Tue, 07/28/2020 - 16:08
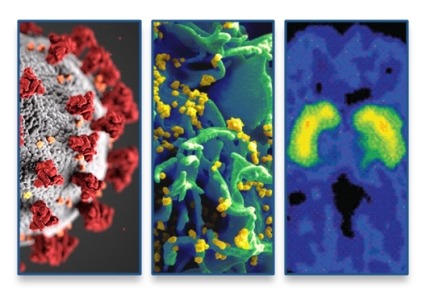
I have written previously about intersections of substance use and substance use disorders (SUDs) with vulnerability to COVID-19 and adverse clinical outcomes. But we also cannot overlook important research on the overlaps of substance use and HIV and AIDS. NIDA and other NIH institutes are using supplementary funds to expand or adapt existing research projects to study the intersection of various health issues with the COVID-19 pandemic. We are prioritizing research into how the coexisting crises of COVID-19, HIV, and substance use, including the opioid crisis, combine to create a disastrous storm, taking lives and overtaxing America’s public health systems.
Research has demonstrated that people with SUDs are at increased risk for acquiring and transmitting HIV, both as a result of sharing injection equipment and because substance use may increase the likelihood of impulsive sex and sex without use of condoms or other HIV prevention tools. For decades, NIDA has devoted considerable resources to support research at the intersection of HIV and substance use. NIDA has the second largest HIV research portfolio at NIH, building unique knowledge related especially to the vulnerable SUD population.
To encourage transformative science and coordinate HIV related research across the institute, NIDA created its AIDS Research Program (ARP) in 2004. In 2008, the ARP established the Avant Garde Awards for HIV/AIDS Research to support individual scientists who propose research relevant to HIV and substance use with high impact potential and that would not typically be funded because of its high risk. In 2015, we launched the Avenir Awards for HIV/AIDS Research to provide grants to early-stage investigators who also propose highly innovative studies.
These commitments to research have led to several significant scientific contributions. A decade ago, NIDA supported a seminal study demonstrating that HIV treatment is prevention, finding that scaling up HIV treatment in people who inject drugs resulted in reductions in community-level viral load and HIV transmission. NIDA-funded research also demonstrated that addiction treatment, especially medications for opioid use disorder, is a necessary part of HIV care and leads to improved viral load, CD4 cell count, and retention in HIV care. A study from NIDA’s Clinical Trials Network found that HIV testing can be integrated into SUD treatment and that counseling offered no additional benefit—findings with broad clinical and public health implications.
The ARP aims also to expand support of basic science research including HIV pathogenesis and the immune response in the presence of addictive substances, including those substances’ ability to promote or interfere with HIV reservoirs in the brain. We are also funding clinical research to develop effective interventions for HIV, substance use, and SUD prevention and treatment, as well as implementation and services research including developing integrated models of care for HIV and SUDs, implementing effective evidence-based practices in routine healthcare settings, and determining the cost and cost-effectiveness of HIV and SUD care. Developing new pre-exposure prophylaxis (PrEP) products to prevent HIV transmission is an ongoing area of research, and NIDA is committed to supporting research to determine feasibility and acceptability of PrEP among people who use drugs.
With additional funds now available to study COVID-19, there is great opportunity for HIV and addiction researchers to make important advances in understanding how COVID-19 intersects with substance use, the opioid epidemic, and HIV. It is already clear that these crises are intertwined and especially impacting vulnerable populations, but many gaps in our understanding remain.
Several co-occurring health problems, including cardiovascular and pulmonary diseases and diabetes, confer greater risk of SARS-CoV-2 infection, severity of disease, and poor outcomes. Additional research could inform us about the clinical impact of COVID-19 on people who use drugs and are living with HIV, as well as the impact that mitigation strategies like social distancing is having on individual health, mental health, and substance use and access to HIV and SUD treatment services. And while knowledge is expanding on how substance use and HIV impact the brain and central nervous system, we know nothing of synergistic short or long-term effects in the presence of COVID-19. There is great potential for knowledge and experience from AIDS care to inform COVID-19 treatment, and conversely, care strategies learned during the COVID-19 crisis could be adapted to HIV outbreaks still seen worldwide that are often connected to injection drug use.
Simply developing effective treatments is no guarantee people using drugs will receive benefit, therefore we cannot expect the development of vaccines or treatments for COVID-19 to confer benefit to this population. When these interventions are available, research will be needed to ensure people using drugs and living with HIV have access. Particularly crucial to study are intersections of HIV, SUD, and COVID-19 among racial and ethnic minority groups, including African Americans, who are consistently disproportionately burdened with poor outcomes across these health conditions. With African Americans suffering and dying from COVID-19 and HIV at higher rates and facing rapidly increasing rates of overdose mortality, research into structural racism and resulting health disparities is more critical than ever. This should include research into stigma within healthcare, which can impede access to care for people of color and those living with HIV and drug addiction.
We cannot forget that in the intense climate of COVID-19, HIV remains a high-priority research area for NIDA. We must develop interventions that are both effective and widely available to address HIV among people who use drugs. The ambitious goal of ending the transmission of HIV will never be realized if we do not also address drug use while ensuring there are no disparities in access to treatment of HIV and SUD.
More information, including funding opportunities, is available through NIDA’s AIDS Research Program.
Comments
Add new comment
The scope of substance use in older adults
While illicit drug use typically declines after young adulthood, nearly 1 million adults aged 65 and older live with a substance use disorder (SUD), as reported in 2018 data.1 While the total number of SUD admissions to treatment facilities between 2000 and 2012 differed slightly, the proportion of admissions of older adults increased from 3.4% to 7.0% during this time.2
Are older adults impacted differently by alcohol and drugs?
Aging could possibly lead to social and physical changes that may increase vulnerability to substance misuse. Little is known about the effects of drugs and alcohol on the aging brain. However, older adults typically metabolize substances more slowly, and their brains can be more sensitive to drugs.3 One study suggests that people addicted to cocaine in their youth may have an accelerated age-related decline in temporal lobe gray matter and a smaller temporal lobe compared to control groups who do not use cocaine. This could make them more vulnerable to adverse consequences of cocaine use as they age.19
Older adults may be more likely to experience mood disorders, lung and heart problems, or memory issues. Drugs can worsen these conditions, exacerbating the negative health consequences of substance use. Additionally, the effects of some drugs—like impaired judgment, coordination, or reaction time—can result in accidents, such as falls and motor vehicle crashes. These sorts of injuries can pose a greater risk to health than in younger adults and coincide with a possible longer recovery time.
Prescription Medicines
Chronic health conditions tend to develop as part of aging, and older adults are often prescribed more medicines than other age groups, leading to a higher rate of exposure to potentially addictive medications. One study of 3,000 adults aged 57-85 showed common mixing of prescription medicines, nonprescription drugs, and dietary supplements. More than 80% of participants used at least one prescription medication daily, with nearly half using more than five medications or supplements,5 putting at least 1 in 25 people in this age group at risk for a major drug-drug interaction.5
Other risks could include accidental misuse of prescription drugs, and possible worsening of existing mental health issues. For example, a 2019 study of patients over the age of 50 noted that more than 25% who misuse prescription opioids or benzodiazepines expressed suicidal ideation, compared to 2% who do not use them, underscoring the need for careful screening before prescribing these medications.6
Opioid Pain Medicines
Persistent pain may be more complicated in older adults experiencing other health conditions. Up to 80% of patients with advanced cancer report pain, as well as 77% of heart disease patients, and up to 40% of outpatients 65 and older.8 Between 4-9% of adults age 65 or older use prescription opioid medications for pain relief.7 From 1995 to 2010, opioids prescribed for older adults during regular office visits increased by a factor of nine.7
The U.S. population of adults 55 and older increased by about 6% between 2013-2015, yet the proportion of people in that age group seeking treatment for opioid use disorder increased nearly 54%.4 The proportion of older adults using heroin—an illicit opioid—more than doubled between 2013-2015,4 in part because some people misusing prescription opioids switch to this cheaper drug.4
Marijuana
Nine percent of adults aged 50-64 reported past year marijuana use in 2015-2016, compared to 7.1% in 2012-2013.10 The use of cannabis in the past year by adults 65 years and older increased sharply from 0.4% in 2006 and 2007 to 2.9% in 2015 and 2016.22
Medical Marijuana
One U.S. study suggests that close to a quarter of marijuana users age 65 or older report that a doctor had recommended marijuana in the past year.10 Research suggests medical marijuana may relieve symptoms related to chronic pain, sleep hygiene, malnutrition, depression, or to help with side effects from cancer treatment.11 It is important to note that the marijuana plant has not been approved by the Food and Drug Administration (FDA) as a medicine. Therefore, the potential benefits of medical marijuana must be weighed against its risks, particularly for individuals who have other health conditions or take prescribed medications.11
Risks of Marijuana Use
Regular marijuana use for medical or other reasons at any age has been linked to chronic respiratory conditions, depression, impaired memory, adverse cardiovascular functions, and altered judgement and motor skills.12 Marijuana can interact with a number of prescription drugs and complicate already existing health issues and common physiological changes in older adults.
Nicotine
The Centers for Disease Control and Prevention (CDC) reports that in 2017, about 8 of every 100 adults aged 65 and older smoked cigarettes, increasing their risk for heart disease and cancer.20 While this rate is lower than that for younger adults, research suggests that older people who smoke have increased risk of becoming frail, though smokers who have quit do not appear to be at higher risk.14 Although about 300,000 smoking-related deaths occur each year among people who are age 65 and older, the risk diminishes in older adults who quit smoking.13 A typical smoker who quits after age 65 could add two to three years to their life expectancy. Within a year of quitting, most former smokers reduce their risk of coronary heart disease by half.13
Nicotine Vaping
There has been little research on the effects of vaping nicotine (e-cigarettes) among older adults; however, certain risks exist in all age groups. Some research suggests that e-cigarettes might be less harmful than cigarettes when people who regularly smoke switch to vaping as a complete replacement. However, research on this is mixed, and the FDA has not approved e-cigarettes as a smoking cessation aid. There is also evidence that many people continue to use both delivery systems to inhale nicotine, which is a highly addictive drug.
Alcohol
Alcohol is the most used drug among older adults, with about 65% of people 65 and older reporting high-risk drinking, defined as exceeding daily guidelines at least weekly in the past year.16 Of particular concern, more than a tenth of adults age 65 and older currently binge drink,18 which is defined as drinking five or more drinks on the same occasion for men, and four or more drinks on the same occasion for women. In addition, research published in 2020 shows that increases in alcohol consumption in recent years have been greater for people aged 50 and older relative to younger age‐groups.21
Risk Factors for Substance Use Disorders in Older Adults
Physical risk factors for substance use disorders in older adults can include: chronic pain; physical disabilities or reduced mobility; transitions in living or care situations; loss of loved ones; forced retirement or change in income; poor health status; chronic illness; and taking a lot of medicines and supplements. Psychiatric risk factors include: avoidance coping style; history of substance use disorders; previous or current mental illness; and feeling socially isolated.19
Alcohol Use Disorder: Most admissions to substance use treatment centers in this age group relate to alcohol.2 One study documented a 107% increase in alcohol use disorder among adults aged 65 years and older from 2001 to 2013.16 Alcohol use disorder can put older people at greater risk for a range of health problems, including diabetes, high blood pressure, congestive heart failure, liver and bone problems, memory issues and mood disorders.16
How are substance use disorders treated in older adults?
Many behavioral therapies and medications have been successful in treating substance use disorders in older adults.
Little is known about the best models of care, but research shows that older patients have better results with longer durations of care.7 Ideal models include diagnosis and management of other chronic conditions, re-building support networks, improving access to medical services, improved case management, and staff training in evidence-based strategies for this age group.7
Providers may confuse SUD symptoms with those of other chronic health conditions or with natural, age-related changes. Research is needed to develop targeted SUD screening methods for older adults. Integrated models of care for those with coexisting medical and psychiatric conditions are also needed.2 It is important to note that once in treatment, people can respond well to care.2
Read more about drug addiction treatment in our Treatment Approaches for Drug Addiction DrugFacts.
Points to Remember
- While use of illicit drugs in older adults is much lower than among other adults, it is currently increasing.
- Older adults are often more susceptible to the effects of drugs, because as the body ages, it often cannot absorb and break down drugs and alcohol as easily as it once did.
- Older adults are more likely to unintentionally misuse medicines by forgetting to take their medicine, taking it too often, or taking the wrong amount.
- Some older adults may take substances to cope with big life changes such as retirement, grief and loss, declining health, or a change in living situation.
- Most admissions to substance use treatment centers in this age group are for alcohol.
- Many behavioral therapies and medications have been successful in treating substance use disorders, although medications are underutilized.
- It is never too late to quit using substances—quitting can improve quality of life and future health.
- More science is needed on the effects of substance use on the aging brain, as well as into effective models of care for older adults with substance use disorders.
- Providers may confuse symptoms of substance use with other symptoms of aging, which could include chronic health conditions or reactions to stressful, life-changing events.
Additional Resources
Learn More
For more information about substance use in older adults, visit:
References
- Substance Abuse and Mental Health Services Administration. (2019). Results from the 2018 National Survey on Drug Use and Health: Detailed tables. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from https://www.samhsa.gov/data/
- Chatre S, Cook R, Mallik E et al. Trends in substance use admissions among older adults. BMC Health Services Research. 2017; 584(17). doi: https://doi.org/10.1186/s12913-017-2538-z
- Colliver JD, Compton WM, Gfroerer JC, Condon T. Projecting drug use among aging baby boomers in 2020. Annals of Epidemiology. 2006; 16(4): 257–265.
- Huhn AS, Strain EC, Tompkins DA, Dunn KE. A hidden aspect of the U.S. opioid crisis: Rise in first-time treatment admissions for older adults with opioid use disorder. Drug Alcohol Depend. 2018 Dec 1; 193: 142-147. doi: 10.1016/j.drugalcdep.2018
- Qato DM, Alexander GC, Conti RM, Johnson M, Schumm P, Lindau ST. Use of prescription and over-the-counter medications and dietary supplements among older adults in the United States. JAMA. 2008 Dec 24; 300(24): 2867-2878. doi: 10.1001/jama.2008.892
- Schepis TS, Simoni-Wastila L, McCabe SE. Prescription opioid and benzodiazepine misuse is associated with suicidal ideation in older adults. Int J Geriatr Psychiatry. 2019; 34(1): 122-129. doi: 10.1002/gps.4999
- Lehmann S, Fingerhood M. Substance-use disorders in later life, N Engl J Med. 2018 December 13; 379(24): 2351-2360. doi: 10.1056/NEJMra1805981
- Galicia-Castillo, M. Opioids for persistent pain in older adults. Cleveland Clinic Journal of Medicine. 2016 June 6; 83(6). Retrieved from: https://mdedge-files-live.s3.us-east-2.amazonaws.com/files/s3fs-public/issues/articles/Galicia-Castillo_OpiodsForOlderAdults.pdf
- Wu LT, Blazer DG. Illicit and nonmedical drug use among older adults: A review. Journal of Aging and Health. 2011; 23(3): 481–504. doi:10.1177/0898264310386224
- Han BH, Palamar JJ. Marijuana use by middle-aged and older adults in the United States, 2015-2016. Drug Alcohol Depend. 2018; 191: 374-381. Retrieved from: https://www.ncbi.nlm.nih.gov/pubmed/30197051
- Abuhasira R, Ron A, Sikorin I, Noack V. Medical cannabis for older patients—Treatment protocol and initial results. Journal of Clinical Medicine. 2019; 8(11): 1819. https://doi.org/10.3390/jcm8111819
- Volkow N, Baler R, Compton W, Weiss S. Adverse health effects of marijuana use. N Engl J Med. 2014 June 5; 370(23): 2219-2227. doi: 10.1056/NEJMra1402309
- Centers for Disease Control and Prevention. Smoking and Older Adults. November 2008. https://www2c.cdc.gov/podcasts/media/pdf/HealthyAgingSmoking.pdf. Accessed March 12, 2020.
- Kojima G, Iliffe S, Jivraj S, Liljas A, Walters K. Does current smoking predict future frailty? The English longitudinal study of ageing. Age and Ageing. 2018 January; 47(1): 126-131. https://doi.org/10.1093/ageing/afx136
- Older adults fact sheet. National Institute on Alcohol Abuse and Alcoholism. https://www.niaaa.nih.gov/alcohol-health/special-populations-co-occurring-disorders/older-adults
- Grant BF, Chou SP, Saha TD, et al. Prevalence of 12‐month alcohol use, high‐risk drinking, and DSM‐IV alcohol use disorder in the United States, 2001‐2002 to 2012‐2013: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiat. 2017; 74(9): 911‐923.
- Kuerbis et al. Substance abuse among older adults. Clin Geriatr Med. 2014 Aug; 30(3): 629–654. doi:10.1016/j.cger.2014.04.008
- Han B, Moore A, Ferris R, Palamar J. Binge drinking among older adults in the United States, 2015-2017. Journal of the American Geriatrics Society. 2019 July 31; 67(10). https://doi.org/10.1111/jgs.16071
- Bartzokis et al. Magnetic resonance imaging evidence of “silent” cerebrovascular toxicity in cocaine dependence. Biol Psychiatry. 1999; 45: 1203-1211.
- Current cigarette smoking among adults in the United States fact sheet. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/data_statistics/fact_sheets/adult_data/cig_smoking/index.htm
- White A, Castle I, Hingson R, Powell P. Using death certificates to explore changes in alcohol‐related mortality in the United States, 1999 to 2017. Alcoholism Clinical and Experimental Research. 2020 January 7; 44(1): 178-187. https://doi.org/10.1111/acer.14239
- Han BH, Sherman S, Mauro PM, Martins SS, Rotenberg J, Palamar JJ. Demographic trends among older cannabis users in the United States, 2006-2013. Addiction. 2017; 112(3): 516-525. doi:10.1111/add.13670
This publication is available for your use and may be reproduced in its entirety without permission from NIDA. Citation of the source is appreciated, using the following language: Source: National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.
Treating Substance Use Disorders Can Reduce HIV Burden in U.S. Cities
mfleming
Wed, 07/15/2020 - 20:56
NIDA Seeks Public Input for Our 2021-2025 Strategic Plan
mfleming
Tue, 07/14/2020 - 14:13
Twice each decade, NIDA (like other NIH Institutes and NIH as a whole) drafts a strategic plan to guide its research and funding decisions. NIDA’s strategic plan is meant to be a high-level articulation of our principles and priorities over the next five years, and how we intend to apply them to capitalize on exciting opportunities or break down research barriers. NIDA has begun drafting its strategic plan for 2021-2025, and to best inform that process, we are seeking input from the public and the scientific community.

The current outline includes elements ranging from basic science to generate knowledge about the brain and how drugs affect it, to clinical, implementation and policy research in healthcare, justice, and other settings. Translational science will accelerate deployment of research findings to inform policy and practice. Specifically, the plan has three main goals:
- Understand Drug Use, Addiction, and the Brain.
- Develop and Test Novel Prevention, Treatment, and Recovery Support Strategies.
- Implement Evidence-Based Strategies in Real-World Settings.
The goals also share three major cross-cutting research approaches identified in the strategic plan outline: leveraging knowledge, technology and innovation, capitalizing on big data analytics and open data sharing, and developing models that capture the real-world complexity of substance use (for instance, use of multiple substances).
We have also identified four topics that straddle multiple goals and that merit specific focus in the years to come: finding ways to reduce the stigma around substance use and use disorders; finding ways to reduce health disparities; understanding sex/gender differences related to substance use and addiction; and understanding the relationships between substance use and other co-occurring conditions like HIV, pain, and mental illness.
The strategic plan is not intended as an exhaustive or prescriptive list of everything NIDA will be doing and funding. NIDA will remain committed to supporting promising research based on investigators’ ideas even when those fall outside these priority areas of focus. But the plan serves as an overarching vision to shape addiction science through our activities over the next five years, as well as a constant reminder of top research topics to address as they appear from our vantage point in the present.
The strategic plan will also have a section outlining how NIDA intends to responsibly steward its public funds over the next five years. Key focus areas including promoting high quality research training and a diverse research workforce, effectively translating and disseminating NIDA-funded research to inform policy and practice, fostering collaboration with public and private partners, supporting the development of a cutting-edge research infrastructure, and doing everything possible to enhance the rigor and reproducibility of scientific evidence.
For more information, including the complete draft outline and instructions for contributing comments, see NIDA’s request for Information (RFI). Again, members of the public as well as the research community are strongly encouraged to respond. Responses are due August 7th to the NIDA Strategic Plan inbox as noted in the RFI.
NOTE: To be considered by the NIDA Strategic Planning Committee, comments must be emailed to NIDAStrategicPlan@nida.nih.gov.
Comments
2021 - 2025 strategic plan
I would like to see the opposition to marijuana legalization relaxed. Admittedly marijuana can adversely affect some people, but the overall benefit to risk ratio is in favor of legalization. The anti-marijuana laws dating back to the 1930s had a racist intent. You may know that William Randolph Hearst the champion of yellow journalism, renamed cannabis marijuana to associate it with Mexicans. Nixon's war on drugs in the early 70's was more of the same. Unless you want to prohibit alcohol again, because it is more dangerous than marijuana, then please get off your high horse and help people make it through their lives with much needed relief from marijuana.
reducing drug addiction
there must be a different approach the NIDA must take to curb drug addiction. Criminalizing addictive drugs may not be the best solution as it leads to a black market environment, organized crime, more potent drugs, a loss of revenue, political corruption, a lack of public understanding of drugs, etc. Ex: the failure of D.A.R.E., the Opium Wars, The 21st century opium trade routes, the development of new drugs after WWI. Yes, all of these events have specific circumstances, but a common element is failed policies to stem a drug considered too horrible by a national government. NIDA should seriously consider advocating politicians to reconsider how we classify drugs.
Marijuana and anxiety
In the work I do, I see marijuana negatively impact young people in their ability to stay in school and cope with normal day to day anxiety. I think we need more research in this area. While I am certain cannabis has medicinal qualities for some disorders, I am highly skeptical that it improves anxiety in any substantial way and in fact, may cause mental health problems. Right now, young people consider it "medicine" for any problem. I think we need to be more clear and specific in this area as I see it destroying many young people who use it daily - especially in concentrated forms. I just think we need more information since this seems to be a wide spread misunderstanding.
2021-2025 Strategic Plan
To protect its own credibility, NIDA should not stand in the way of legalizing cannabis, especially medical cannabis.
And funding should go to research intended to confirm potential benefits of cannabis as well as research aimed at finding harm.
To put it bluntly, the government has lied about cannabis for decades and you have played a significant role in this deception. This is shameful for a medical organization.
As Sanjay Gupta, M.D., acknowledged: “I mistakenly believed the Drug Enforcement Agency listed marijuana as a schedule 1 substance because of sound scientific proof. Surely, they must have quality reasoning as to why marijuana is in the category of the most dangerous drugs that have “no accepted medicinal use and a high potential for abuse.” They didn’t have the science to support that claim, and I now know that when it comes to marijuana neither of those things are true. It doesn’t have a high potential for abuse, and there are very legitimate medical applications. In fact, sometimes marijuana is the only thing that works. We have been terribly and systematically misled for nearly 70 years in the United States, and I apologize for my own role in that.”
2021-2025 Strategic Plan
The National Institute of Drug Abuse has a consistent record of funding and promoting biased research that portrays cannabis in a negative light, despite numerous large-scale and controlled studies showing the contrary. The LaGuardia Committee and the American Medical Association both denounced cannabis criminalization, citing that it does not lead to addiction nor is it a gateway drug. On the contrary, recent studies show the ability of cannabis to help individuals reduce or cease use of opioids, sleep medications, tobacco, and other street drugs such as cocaine. NIDA's insistent efforts to fund research on Cannabis Use Disorder is based on a fallible, correlation-based theory about the motivation behind cannabis use and is against the best interests of a population struggling with an opioid epidemic.
The REAL Harms of Marijuana - Prohibition
Science and widespread experience have shown marijuana is not addictive and is far less harmful than alcohol. - Yet, more than 600,000 innocent Americans are arrested for simple marijuana possession each year and made second-class citizens - for life!
They will forever face large obstacles to decent employment, education, travel, housing, government benefits, and will always go into court with one strike against them. They can even have their children taken away!
25 million Americans are now locked away in this very un-American sub-class because of this bogus "criminal" record. That has a horrible effect on the whole country, being a massive waste of human potential.
The fraudulent marijuana prohibition has never accomplished one positive thing. It has only caused vast amounts of crime, corruption, violence, death and the severe diminishing of everyone's freedom.
There is no more important domestic issue than ending what is essentially the American Inquisition.
Soy ex- consumidor, 58 años,…
Soy ex- consumidor, 58 años, terminando de estudiar , Tecnico en rehabilitacion de adicciones, en Universidad de Santiago de Chile
Vivo en Chile, Y deseo compartir experiencia vivida.
Saludos Sebastian Braniff
Opioids
Each individual has a different tolerance to pain medication. Roux En Gastric Bypass patients can't have any kind of NSAIDs. Tylenol products only 4000 mg a day is not enough for a Failed Total knee replacement. Each person might need tested in medication that will work instead of wasting the doctor & patients time & insurance money. No one should have to suffer any kind of pain!
Drugs
Drugs are not illegal because they are dangerous they are dangerous due to the lack of regulation (like drinking what you think is a pint of lager, turns out it's really moonshine) Carnage! Crime generates money, legalizing drugs would vastly cut crime and greatly reduce profit for the greedy at the top. Its high time somebody took responsibility we should be using our get it sorted.. the law against drugs is ludicrous its immoral and bullying
Youth & Marijuana
I am a teacher by background. The brains of our youth are the most precious natural resource we as a nation have. I now add - TO PROTECT.
Countless studies show that prevention gets a very minor slice of the drug addiction expenditure finances.
How about funding a study that shows the effects of requiring all teachers, after school programs, school personnel, school administrators, school sports coaches, school PTO groups, school boards, and community organizations working with youth to have a well orchestrated program showing the harms of high potency marijuana, frequent marijuana use, and the gateway drug effect to meth, opioids, even alcohol with and awareness of programs like Iceland's and really see if this approach doesn't make an impact on all of the other reduction plans you fund.
Be sure to include preganant mothers and preschools, headstart, and daycare providers.
Martha Hafner
Vermont
PS I am 30+ years a teacher and I do have some resources that could serve as a boiler plate.
Moratorium on funding studies on THC/CBD Pregnancy
Due to the overwhelming scientific research that supports the conclusion that the use of marijuana in pregnancy poses significant risks to the offspring as well as mothers to be there should be a moratorium on federal funding of any research or study that involves recruiting women who are using THC/CBD in pregnancy for any reason. The Surgeon General has issued statements about the evidence of harm from prenatal use of this drug and therefore no women should be enrolled in any research that seeks to study the results of the impact of use on maternal health or offspring and no research should be granted federal funds that can be used in any way to support the erroneous argument that we do not know the result of marijuana use in pregnancy as the evidence is now conclusive enough to continue to warn all women not to use CBD or THC when planning or starting a family.
This moratorium on any studies designed to recruit pregnant women who use marijuana is further supported by the Helsinki Declaration and The Belmont Report and the articles that govern research on human subjects. The research in animal studies does not show safety and therefore prenatal marijuana studies breach international human rights legislation.
strategic plan re: psychoactive sub abuse
Unresolved early trauma needs to be addressed. Extended care is crucial and motivational enhancement is vital to client engagement for at least 18 months. And we recognize that most clients abuse multiple agents.
Rich
The "Treatment" for this…
The "Treatment" for this disease CAN'T be the same 12 steps one guy thought of in the 1930's.... That is not treatment, it's insanity.....
And it's also a big problem that the 10% of people it does work for, spend their life convincing vulnerable people that it is an answer..... It's wreckless, it's dangerous, and it's accepted for some reason....
Add new comment
Marijuana Concentrates DrugFacts
amartinek
Thu, 06/25/2020 - 13:06
Cannabis plants are covered by microscopic, mushroom-shaped, hair-like compounds called trichomes. These outgrowths surround the budding marijuana flower and produce the plant’s cannabinoids. Different varieties of trichomes can be collected. The resulting products—collectively called cannabis concentrates—can contain very high levels of tetrahydrocannabinol, commonly referred to as THC, the psychotropic ingredient in marijuana. These THC-rich marijuana products may be vaporized and inhaled using a vape pen or through a process called dabbing.1
How are concentrates made?
Marijuana concentrates can be made in a commercial environment with modern equipment or prepared in a home setting.2 They are produced in various ways, including:
- dry processing (kief, finger hash)
- dry ice processing
- water-based processing (bubble hash)
- combining pressure with heat
- using nonflammable carbon dioxide solvents
- using flammable solvents, including butane (lighter fluid), propane, ether or alcohol1
Using flammable solvents is popular because the products have high THC levels,1 users report longer-lasting effects,1 and it is a relatively inexpensive and efficient production method.2 Butane is a commonly used solvent, producing the potent marijuana concentrate butane hash oil (BHO), also known as amber, dab, glass, honey, shatter, or wax.2
What does the final product look like?
The products resulting from these methods may be:
- a gooey liquid wax (hash oil or honey oil)
- a soft solid with a texture like lip balm (wax or budder)
- a hard, amber-colored solid (shatter)
Hash oil and waxes can be consumed using vape pens. Solids can also be placed on a heated platform usually made of titanium, quartz, or ceramic, where they are vaporized by high heat and inhaled through a dabbing tool, often called a rig.2
What’s the difference between concentrates, extracts, and dabs?
The terms used to describe these products vary. Concentrates is a broad term referring to all products that have been extracted from the plant. Although extracts and concentrates are often used interchangeably, some people define extracts as products manufactured using solvents, but not those pulled from the plant with non-solvent methods. Dabs may refer to products made exclusively from butane hash oil; however, the term is sometimes used colloquially for concentrates extracted in other ways. There are also post-production methods that lead to further variations in products and terms.3
What are the health effects of concentrates?
There are adverse effects associated with marijuana use in any form,3 though additional research is needed to understand how the use of concentrate may differ from smoking dried marijuana buds. Marijuana concentrates have very high levels of THC. Solvent-based products tend to be especially potent, with THC levels documented at an average of about 54-69% and reported to exceed 80%, while non-solvent based extraction methods produce average THC levels between 39-60%.4 In comparison, the THC content in marijuana plant material, which is often used in marijuana cigarettes, is lower—with samples seized by the U.S. Drug Enforcement Agency averaging just over 15%.5 Not only do concentrates have high levels of THC, but dabbers inhale the entire amount all at once—in a single breath.2 As a result, concentrates can deliver extremely large amounts of THC to the body quickly. The risks of physical dependence and addiction increase with exposure to high concentrations of THC, and higher doses of THC are more likely to produce anxiety, agitation, paranoia, and psychosis.6 Additional research is needed to understand how the use of concentrate affects these risks.
In addition, contaminants in concentrate products may be cause for concern. One study noted that 80% of tested concentrate samples were contaminated in some form, not only with pesticides (which is also a concern for dried bud), but also with residual solvents that were not fully purged in the manufacturing process. Users of BHO, for example, likely inhale some butane and other impurities along with the vaporized THC.2 It is important to note that direct inhalation of concentrated butane among recreational inhalant users carries multiple risks, including reported deaths.7 However, it is unclear what negative health outcomes result from the inhalation of residual butane, other solvents, or leftover contaminants during the dabbing process.
Is it dangerous to make solvent-based concentrates?
When solvents are used to produce concentrates, the preparation process itself can be dangerous. A number of people using butane to make extracts at home have caused fires and explosions and have been seriously burned.8 A study conducted in 2015 looking at implications from marijuana legalization in Colorado reported that in a 2-year period the University of Colorado burn center saw a substantial increase in the number of flash burns that occurred during amateur THC extraction using butane, some involving more than 70% of body surface area and most requiring skin grafting.9
It is against federal law to manufacture BHO,10 and even in some states where adult use of marijuana is legal, like Colorado and California, it is illegal to make hash oil using flammable liquids. In Colorado, state officials recommend alternate methods using nonflammable dry ice (CO2), ice water, or purchasing the product from a licensed marijuana retail store.11 Most licensed, commercial production facilities use a safer extraction system that prevents solvents from being wasted or exposed to the open air where they could inadvertently be ignited, similar to decades-old systems used in the production of many commercial products.2
Points to Remember
- Cannabis plants are covered by microscopic, mushroom-shaped, hair-like compounds called trichomes which surround the budding marijuana flower and produce the plant’s cannabinoids.
- Trichomes can be collected and made into concentrates, including extracts and dabs.
- Concentrates can contain very high levels of THC, the psychotropic ingredient in marijuana.
- Concentrates can be vaporized and inhaled using a vape pen or by dabbing.
- Concentrates can be made in commercial settings or in a home through several methods, including dry ice- and water-based processing and the use of solvents.
- Using flammable solvents, such as butane, propane, ether or alcohol, is popular because it produces high THC levels, longer-lasting effects, and it’s relatively inexpensive.
- Using butane as a solvent produces the potent marijuana concentrate butane hash oil (BHO), also known as amber, dab, glass, honey, shatter, or wax.
- Exposure to high levels of THC increases the risks of physical dependence and addiction. Higher doses of THC are more likely to produce anxiety, agitation, paranoia, and psychosis.
- Contamination with pesticides and residual solvents that weren’t fully removed during production is a concern. People who use BHO likely inhale some butane and other impurities along with the vaporized THC.
Learn More
For more information about marijuana and marijuana use visit
References
- Raber JC, Elzinga S, Kaplan C. Understanding dabs: Contamination concerns of cannabis concentrates and cannabinoid transfer during the act of dabbing. J Toxicol Sci. 2015;40(6):797-803. doi: 10.2131/jts.40.797
- Al-Zouabi I, Stogner JM, Miller BL, Lane ES. Butane hash oil and dabbing: Insights into use, amateur production techniques, and potential harm mitigation. Subst Abuse Rehabil. 2018;9: 91–101.
- Volkow ND, Baler RD, Compton WM, Weiss SRB. Adverse Health Effects of Marijuana Use. N Engl J Med. 2014;370(23): 2219–2227. doi:10.1056/NEJMra1402309.
- Meier MH, Docherty M, Leischow SJ, Grimm KJ, Pardini D. Cannabis concentrates use in adolescents. Pediatrics. 2019;144(3):e20190338. doi:10.1542/peds.2019-0338.
- National Institute on Drug Abuse. Is marijuana addictive? drugabuse.gov. https://www.drugabuse.gov/publications/research-reports/marijuana/marijuana-addictive. Updated April 8, 2020. Accessed June 17, 2020.
- Freeman TP, Winstock AR. Examining the profile of high-potency cannabis and its association with severity of cannabis dependence. Psychol Med. 2015;45(15):3181-9. doi: 10.1017/S0033291715001178.
- Sironi L, Amadasi A, Zoja R. Recreational inhalation of butane and propane in adolescents: Two forensic cases of accidental death. Forensic Sci Int. 2016;266:e52-e58. doi: 10.1016/j.forsciint.2016.05.028.
- Romanowski KS, Barsun A, Kwan P, et al. Butane hash oil burns: A 7-Year perspective on a growing problem. J Burn Care Res. 2017;38(1):e165-e171. doi: 10.1097/BCR.0000000000000334
- Monte AA, Zane RD, Heard KJ. The implications of marijuana legalization in Colorado. JAMA. 2015;313(3):241-2. doi: 10.1001/jama.2014.17057.
- Two charged in connection with drug lab explosion. dea.gov. https://www.dea.gov/press-releases/2018/09/06/two-charged-connection-drug-lab-explosion. Published September 6, 2018. Accessed June 17, 2020.
- Safety with hash oil. Colorado.gov. https://www.colorado.gov/pacific/marijuana/safety-hash-oil. Accessed June 17, 2020.
This publication is available for your use and may be reproduced in its entirety without permission from NIDA. Citation of the source is appreciated, using the following language: Source: National Institute on Drug Abuse; National Institutes of Health; U.S. Department of Health and Human Services.
Office of Research Training, Diversity, and Disparities (ORTDD)
What We Do
The Office of Research Training, Diversity, and Disparities (ORTDD) offers a wide range of programs, workshops, and funding mechanisms to support the development of substance use and addiction research scientists throughout the career pipeline. The ORTDD is committed to providing training opportunities to ensure a cutting-edge diverse research workforce that will advance the knowledge base needed to address urgent public health substance use and addiction problems.
Offices within the ORTDD
The Office of Research Training and Career Development (ORT)
The Office of Research Training and Career Development (ORT) provides research grants to promising scientists to meet the Nation’s need for drug abuse and addiction research. NIDA’s portfolio includes research in basic, clinical, and translational sciences. Read more about the NIDA ORT career development fellowships and grants.
Introduction to Research Training at NIDA
NIDA offers a strategic set of funding mechanisms to support the development of research scientists through multiple stages of their careers. These awards are designed to ensure that scientists of the very highest caliber are available to meet the Nation’s need for substance use and addiction research. NIDA’s portfolio includes research in basic, clinical, and translational sciences. This includes genetics, epigenetics, molecular biology, neuroimaging, cognitive and social neuroscience, pharmacological and behavioral therapies, prevention, epidemiology, health services, health disparities, HIV/AIDS and other related domains. NIDA also promotes opportunities for quantitative scientists from fields such as mathematics, bioengineering, and physics to apply their knowledge to the study of substance use and addiction.
The Office of Diversity and Health Disparities (ODHD)
The Office of Diversity and Health Disparities (ODHD) offers programs to help undergraduate and graduate students, postdoctoral fellows, and early-stage investigators from underrepresented backgrounds launch their independent research careers. NIDA aims to enhance the representation of these scientists in the biomedical research workforce through outreach, education, and other research training initiatives. Read more information about NIDA ODHD programs and initiatives.
What We Do
To enhance the pool of underrepresented populations in the sciences, the National Institute on Drug Abuse established the Office of Diversity and Health Disparities (ODHD) 20 years ago. The mission of the ODHD is to strengthen the NIDA extramural research portfolio through a more diverse and robust extramural research workforce, attracting and retaining talented individuals from all populations in order to fulfill the mission of NIDA. The ODHD’s goals are to:
- Promote and support underrepresented scholars and researchers actively participating in research;
- Enhance the pool of underrepresented scholars and researchers independently funded to conduct substance abuse research;
Ensure that research addressing health disparities is adequately represented in NIDA’-supported substance abuse research.
Underrepresented researchers face a number of challenges that influence their success in obtaining independent support from NIDA, the NIH, and other federal funding agencies. Some of these challenges include limited/poor mentoring, lack of adequate knowledge of NIH funding opportunities and processes, limited access to novel high priority research projects and design, low publication records, and limited professional networking to successfully bridge to the next career level. Collectively, these factors impact NIDA's efforts to retain underrepresented investigators conducting substance abuse research and further develop the research infrastructure within this community. To that end, NIDA has implemented several key early stage outreach programs which play a vital role at recruiting, training, and retaining underrepresented researchers from underrepresented backgrounds in order to develop and support their research careers.
area
Wed, 06/24/2020 - 12:04
NIDA Researchers Adapt Their Projects to Study COVID-19
mfleming
Mon, 06/15/2020 - 21:54
The U.S. is now facing two intersecting health crises, the ongoing opioid overdose epidemic and the COVID-19 pandemic. Regrettably, each has the potential to exacerbate the effects of the other. In March, NIDA released a Notice of Special Interest to alert researchers with existing grants to our interest in supporting applications for administrative supplements and urgent competitive revisions that could be used to investigate aspects of COVID-19 as they intersect with substance use and related areas in NIDA’s research portfolio, like HIV. These applications are being reviewed on a rolling timeline (and we will continue to update this blog as new supplements are awarded).
NIDA has thus far issued nearly $4 million in funding for COVID-19-related projects that could leverage current infrastructure, projects, or scientific knowledge and resources. Those projects range from assessing the virus’s impact on individuals with a substance use disorder (SUD), including those who are homeless or incarcerated, to basic research to investigate potential interactions between drugs and COVID-19, including effects on the immune system. At the same time, researchers at NIDA’s Intramural Research Program (IRP) quickly responded to the pandemic with new ideas to exploit their knowledge and research capabilities.
Since substance use may put people at increased risk for infection with SARS-CoV-2 or the most serious outcomes of COVID-19, several research projects will be assessing this. Smoking and vaping—both of nicotine and cannabis—may be risk factors for worse COVID-19 outcomes, so we are funding supplements to examine COVID-19 in people who smoke and/or vape. A project at Boston University will use single-cell transcriptomics (a method to study gene expression via RNA) to examine whether smoking and vaping are risk factors for severe COVID-19 and its associated cytokine storm—an immune response that proves fatal in some patients. Researchers at the University of Tennessee-Knoxville studying the effects of text-messaging-delivered peer network counseling in young adults with cannabis use disorder will use supplemental funding to examine the impact of COVID-19 on health, smoking/vaping, and other substance use behaviors in this population.
The NIDA-funded National Drug Early Warning System (NDEWS) is a network of researchers at 18 sites across the country collecting and sharing data on drug use trends. With new supplemental funds, NDEWS will be expanding its efforts to track substance-use-related COVID-19 consequences in several urban, rural, and suburban areas with the help of local informants including funeral directors, emergency medical technicians, and staff at syringe services programs, to rapidly share the information gathered.
NIDA-funded researchers at the University of California-San Diego are looking at social networks, drug markets, and drug tourism among people who inject drugs in San Diego and Tijuana. Supplemental funds will enable them to expand their study to test this population for SARS-CoV-2 infection using nasal and fecal samples. This data will provide information about transmission of the virus among people who use drugs on both sides of the US-Mexico border and potentially inform policymakers about the impact of proposed mitigation strategies such as closure of the border.
Social distancing to prevent the spread of the coronavirus may lead to more individuals using drugs alone, raising the risk of overdose because bystanders may not be present to intervene or may be reluctant to intervene. Another project by researchers at New York University will study the effects of COVID-19 on opioid overdose risk behavior and how it is affecting access to and use of naloxone. The need for social distancing has increased the use of telemedicine and has resulted in the relaxation of rules governing the dispensing of controlled medications like methadone and buprenorphine. Building on their ongoing study of HIV/hepatitis and opioid prevention and treatment, supplemental funds will allow researchers at Oregon Health and Science University to examine how opioid treatment programs are implementing the new policy allowing four weeks’ worth of take-home doses of methadone for stable patients (and two weeks’ worth for others, based on clinics’ discretion), as well as assess the effects of this change. The researchers will also analyze Medicaid claims to study COVID-19 diagnoses and estimate treatment burden among people with opioid use disorder.
Social distancing has also made it harder to access behavioral treatment and recovery supports.
NIDA research has already supported numerous devices and apps to help people with SUD connect virtually to peers and counselors, and some startups are adapting their innovations to address the COVID-19 crisis. Researchers at the University of Wisconsin-Madison are using a NIDA supplement to adapt their ACHESS smartphone recovery app to help users with social distancing, adjusting to isolation, and using virtual SUD treatment and recovery services. They will also assess the impact of their app on users’ anxiety, loneliness, and reported COVID-19 infections.
An ongoing study by NIDA IRP researchers finding ways to measure psychosocial stress in people receiving treatment for OUD is being modified to allow participants to complete questionnaires and answer questions online rather than visiting a clinic or physically engaging with research staff. This will enable the researchers to measure the impact of COVID-19 on recovery, relapse, and medication adherence in this group.
Several projects are also looking at COVID-19 as it relates to HIV. Using supplemental funds to their existing grant to study implementation of pre-exposure prophylaxis for HIV prevention (PrEP) among people who inject drugs, researchers at Boston University Medical Campus will interview clients and staff of syringe-service programs to assess the impact of COVID-19 on drug markets, HIV-risk behaviors, use of HIV prevention services, and the way those services have adapted to the pandemic.
Two projects, one at the University of Maryland, Baltimore, and another at Massachusetts General Hospital, will also examine how underlying HIV infection affects COVID-19 disease progression in people who use opioids. A project at Johns Hopkins University will study barriers to receiving drug treatment and HIV/HCV care caused by the requirements of social distancing during the COVID-19 pandemic. And a study by researchers at the University of Miami School of Medicine will examine whether there are synergistic associations of methamphetamine use and HIV with SARS-CoV-2 prevalence in men who have sex with men.
Another especially vulnerable population is mothers and their children, in part because of limited access to health services during the pandemic. Researchers at Oklahoma State University for Health Sciences who are doing a feasibility study related to the proposed HEALthy Brain and Child Development (HBCD) study will use supplemental funds to assess the ability of pregnant women and new mothers (both with and without a history of SUD) to access treatment and mental health services during the COVID-19 crisis. Researchers at seven other sites across the country who are already recruiting pregnant and postpartum women for the HBCD study will also examine COVID-19’s impact on birth outcomes, parenting stress, and early childhood developmental milestones.
Researchers in the ABCD Study, now in its third year of data collection, will also leverage their infrastructure by surveying participating children and their parents about the impact of COVID-19 and the associated social, behavioral, and economic impacts on multiple aspects of their lives. A subset of children (N=500) who were issued Fitbits prior to the COVID-19 shutdown of schools and research site visits, continue to wear their devices so that information about their physical activity and sleep before, during, and after pandemic can be studied and compared.
Basic research supported by NIDA could also contribute to the development of new treatments for COVID-19. The Coronavirus-2 spike protein is known to bind to human angiotensin converting enzyme 2 (ACE2) receptors, and this is the focus of multiple investigations. A two-year project by researchers at Icahn School of Medicine at Mount Sinai will seek to identify molecules that could block this interaction, keeping the virus from invading host cells; they will also screen potential COVID-19 medications for interactions with medications used to treat SUD. A lab at NIDA’s IRP in Baltimore will also study the SARS-CoV-2 spike protein’s binding and affinity for various human cell types and test possible molecules that could be therapeutically useful.
A team at Scripps-Howard Research Institute has already developed a type of therapeutic agent (aminoadamantane nitrates) that has a protective effect on the neurons of people with Alzheimer’s disease and of people with HIV who use methamphetamine. These agents show activity in the ion channel in the envelope of the SARS-CoV-2 virus and may be able to enter it, so these compounds will be tested as possible molecular “warheads” to disrupt viral activity. Since viruses can cause damaging stress responses in a cellular structure called the endoplasmic reticulum, another laboratory at the NIDA IRP will test the effects of FDA-approved and novel drugs that might modulate these responses in the context of SARS-CoV-2 infection.
Pandemics are devastating, and COVID-19 is proving to be no exception, coming while America is already in the midst of the opioid crisis. But we now live in a world where science can be quickly mobilized to find solutions to mitigate its worst effects. Along with the other Institutes and Centers of the NIH, NIDA has swiftly responded to the COVID-19 crisis by supporting research in areas of basic science, prevention, treatment, epidemiology, and implementation, particularly at the intersection with SUD. I am hopeful that these supplemental funds will contribute to lessening the impact of the collision between the opioid and COVID-19 crises.
Add new comment
A Message from the Director on Racially Motivated Violence
jlinton
Thu, 06/04/2020 - 09:44

This is a painful week in the United States as we again confront the systemic racism that has plagued our country since its founding. Listening to the conversation on racism taking place right now in response to the recent violent deaths of African Americans is critical, and I encourage readers to hear what Black/African Americans are saying about their experiences.
NIH’s mission is to seek fundamental knowledge about the nature and behavior of living systems and the application of that knowledge to enhance health, lengthen life, and reduce illness and disability. Science has told us repeatedly that systematic, widespread discrimination of Black/African-American people is diametrically opposed to these aims, and what’s more, it is unacceptable and wrong.
The long history of discrimination against racial minorities in America bears directly on NIDA’s mission to address addiction as a disease rather than a moral failing to be dealt with through punishment. Whites and Black/African Americans use drugs at similar rates, but it is overwhelmingly the latter group who are singled out for arrest and incarceration. This use of drug use and addiction as a lever to suppress people of a particular race has had devastating effects on communities of color.
We know that science itself is at its best when it is most inclusive, and humans are best when we embrace diversity. Conversations about systemic racial inequalities can be uncomfortable but are clearly needed. Entrenched, systemic, pervasive racism is perpetuated by silence, and we cannot let it continue. I look forward to working with the addiction science community – researchers, the medical community, law enforcement, advocates, policymakers, other stakeholders and the public – to eradicate discrimination and promote equality.
Nora D. Volkow, M.D.
Director
Comments
racial predjudice and blatant discrimination
At the genetic level, all humans are highly concordant. Diversity promotes a much richer human experience. However, due to partisan politics all this is occurring within the deteriorating US Incivility War. Under these circumstances our challenge is even greater.
Rich
Message from the Director
Thank you Dr. Volkow ~ We needed to hear from you. I am with you every step of the way, as I am sure all of us in this field must be. We all need to Stand Up and Speak Up. In Peace and Health, Teri
NIDA's role & complicity in perpetuating racial injustice.
Dr. Volkow,
Thank you for using your platform to draw attention to the discriminatory enforcement of America's anti-drug policies. While we appreciate your acknowledgement that these policies are applied in a prejudicial manner, it's quite disappointing that you were unable—or unwilling—to acknowledge that much of this sad reality can be attributed you and NIDA's actions.
The public looks to you as a leader. When you make statements like "yes, tobacco is more harmful for cancer—but marijuana is more harmful as it disrupts who you are as a person", you're actively perpetuating a nearly century long history—which was actively planned and perpetuated by US bureaucrats and politicians—of using marijuana consumption as a racist and xenophobic dogwhistle.
Even if one were to ignore the fact that "harming your humanity" is not a valid scientific concept, the fact that you've used your tremendous influence to engage in fear-mongering and traffic in racist stereotypes is shameful. I encourage you to spend some time learning about the pernicious role racism played in drug policy (not just drug policy enforcement), reckon with the harms you've helped to perpetuate, and work to start making amends.
Thank you.
The concept of racism virus
Racism is a socially transmitted disease from generation to generation, and it has evolved and it is evolving. The racism virus is causing a pandemic of racism, and there is no treatment, and cannot be stopped. Racism like addiction is a disease.
Racism Today
Thank you Dr Volkow!!
Access to Newsletter
Our researchers here at THCBD LLC (NJ based BioTech startup) agree 100% with Dr. VolKow's comments. Furthermore will we would like to point out that allowing Cannabis Sativa L. to say as a Schedule I Drug is a prohibition against science.
Schedule I does not allow cannabis researchers to advance cannabis science.
De-Schedule now!
All the best, Gaetano Lardieri, Cannabis Advocate and Entrepreneur, Founder THCBD LLC
So apropos- the fundmental problem is DRUGS!
Wholehearted agreement- just some issues with paragraph three.
Likely ‘classism’ more-so than racism is what haunts us. Economic growth can be an amazing antidote.
Addiction per se is not a crime! Treat addiction as a disease. Yes, Blacks and Whites use illicit drugs at similar rates. But arrest and incarceration derive from serious crimes- like robbery with dangerous weapons, vandalism, assault, drug dealing, repeat offenses, etc. Black Americans seem disproportionately arrested because cops are called to areas of real street crimes- which unfortunately happen to be disadvantaged communities. Let’s dispel the “marijuana possession mass incarceration” hoax.
Why is there so much violent crime in the inner cities? It’s DRUGS! Read news articles, police reports, etc; the connection to our drug culture is astonishing! Dealing, addiction, mental illness, whatever- many are simply not in their right minds. They rob, steal, resist arrest, carry weapons. Police will necessarily be harsh- with ANY ethnicity. BLM and the media cherrypick for political purposes.
Where is the drug demand? Turns out with some research and common sense, liberal/progressives (not monolithically) provide the disposable income and the demand that allows our drug culture to thrive! They’re the financiers of the veritable Latin American drug holocaust (seems racist to me), environmental destruction, the catalyst behind the opioid crisis, violence across America (drug gangs), ambush/murders of cops and the tragedy of the inner cities.
Let’s not be silent any more, be courageous and address the great American drug tragedy caused primarily by the progressive left.
Gracias
I often read their messages and interview. In this last message, you reveal one of the several ill-intentioned open and covert goals of drug trade and use. Thank you.
I love Nora Volkow
I love this woman. Historical perspective and a social conscience in a research scientist. I love Her. I love her. I love her.
MAT Treatment
Hello Dr. Volkow. I own an addiction treatment center in southern California. A portion of our counselors and some therapists are firm believers in the 12-Step abstinence model of addiction treatment, and... to be honest... they are not very open to MAT... Can you recommend some consultants that I can retain to help educate my resistant Clinical team ?
NIDA’s website has materials…
NIDA’s website has materials that show the crucial importance of medications in treatment for opioid addiction, including this: https://www.drugabuse.gov/publications/effective-treatments-opioid-addiction
The 2019 report by the National Academies of Science, Engineering, and Medicine, “Medications for Opioid Use Disorder Save Lives,” presents the evidence comprehensively: https://www.nap.edu/catalog/25310/medications-for-opioid-use-disorder-save-lives(a free pdf is available on that page).
Nora's Blog - Words Matter
Thank you Nora for writing about the importance of using terminology that helps avoids stigmatizing persons with addiction. As a professional working with addiction, I couldn't agree more.




NIDA Research
on August 3, 2020
I have been in this field for over 50 years. The investment the taxpayer has made in NIDA research is quite disappointing to me. Prevention - the drug abuse problem is worse than ever and the strategies for prevention have not been successful, Treatment - the only curriculum supported by NIDA is the Matrix, we do have evidence-based treatment, not sure NIDA has had much to do with it. MAT - the sole focus on opiates and the lack of recognition of methamphetamine as the primary drug of choice and problem in the western part of the country and on the reservations is a big hole that NIDA should have focused on and now we are in no-man's land. Great disappointment. In fact, the focus on HIV, MAT and Opiates has been a big disappointment (what MAT drugs work best with which opiate clients - who should be on MAT and who doesn't need it) while other areas like prevention, methamphetamine MAT and related treatment, Native American treatment effectiveness, and effective recovery strategies have been sorely neglected. The direction of management at NIDA for the research dollar is very questionable. The gains made for all the money spent on biological research is minimal.
Just my thoughts.