
This was originally published in a 2019 National Association of Social Workers’ Alcohol, Tobacco and other Drug specialty section newsletter.
The most striking thing about substance abuse treatment is the mismatch between the duration of treatment and the duration of the illness.
—Robert DuPont, MD 1DuPont R. (March, 2018) Interview with Brian Coon. Interview presented at the NC Recovery Alliance Summit, Durham, NC.
The opioid crisis has shined a spotlight on the U.S. addiction treatment system. Much of the coverage has focused on profiteering, the failure of states to reform their systems, the failure of programs to adopt evidence-based practices, and exploitation of patients. Many of these criticisms are well-deserved and have the potential to create opportunities to discuss how the addiction treatment system should be designed. Social workers need to involve themselves in this discussion to assure that the needs of vulnerable patients are considered and our values and priorities are represented.
Several unique qualities of the opioid crisis (its lethality, its frequent iatrogenic origins, and the availability of pharmacological treatments) have raised important questions about treatment-as-usual representing a one-size-fits-all approach. It could be argued that the responses to these questions have been debates about which one-size-fits-all approach—inpatient, agonist, partial agonist, antagonist, harm reduction—should prevail. Social work’s emphasis on families, communities, social functioning and overall well-being provides a unique perspective. Where others are interested in reducing social costs, reducing medical costs, reducing symptoms, reducing crime and reducing disease transmission, we’re interested in all of those outcomes and maximizing the wellness of individuals, families and communities.
If we focus on maximizing individual wellness, a few models stand out. Professional monitoring programs for impaired pilots, lawyers and health professionals have very good outcomes and focus not just on the amelioration of symptoms, but also outcomes like returning to work. The most well-researched of these programs are physician health programs (PHPs). A large and long study of 904 physicians in 16 states reported the following 5-year outcomes 2DuPont RL, McLellan AT, White WL, Merlo LJ, Gold MS. (2009), Setting the standard for recovery: Physicians’ Health Programs. J Subst Abuse Treat. 36(2):159-71. Doi: 10.1016/j.jsat.2008.01.04.:
- 78% of participants had no positive test for either alcohol or drugs;
- Of those who experienced a relapse, only 22% had a second relapse;
- Participants averaged 83 drug tests over a mean period of 54 months;
- 72% of participants were retained in the monitoring program;
- 72% of participants were still employed as physicians;
- Outcomes did not differ by primary substance (alcohol, cocaine, opioids) or whether they injected drugs.
It’s important to note that this study reported on 5 year outcomes, monitored alcohol and other drug use, and reported on an important quality of life measure (return to employment). This represents a rare level of rigor.
What does this program consist of? The study proposed the following elements as the essential ingredients of the model:
- Contingency management
- Frequent drug testing
- Active linkage to abstinence-oriented mutual aid groups
- Active management of relapse with intensified treatment and monitoring
- Continuing care that lasts 5 years
- Focus on lifelong recovery
Most readers will wonder whether these program outcomes are relevant to the general population. Objections typically fall into three categories.
The most common objections tend to focus on the doctors as a cohort with unusually high levels of recovery capital (the quantity and quality of internal and external resources that one can bring to bear to initiate and sustain recovery from addiction) 3Laudet AB, White WL. (2008). Recovery capital as prospective predictor of sustained recovery, life satisfaction, and stress among former poly-substance users. Subst Use Misuse. 43:27–54.. To be sure, there may be ways in which health professionals are unique in terms of recovery capital. However, they also face a unique set of barriers when initiating recovery. Another PHP study 4DuPont RL, McLellan AT, Carr G, Gendel M, Skipper GE. (2009), How are addicted physicians treated? A national survey of Physician Health Programs. J Subst Abuse Treat. 37(1):1-7. found high rates of opioid addiction (35%), high rates of combined alcohol and drug problems (31%) and high rates of psychiatric problems (48%), and 74% were not self-referred. Further, health professionals have easy access to drugs and often develop tolerance levels that eclipse those of street addicts.
Two pieces of folk wisdom may also be relevant. First, it’s often said that doctors make the worst patients. Second, a common joke in treatment and recovery circles is, “I’ve never met anyone too simple-minded for recovery, but I’ve met plenty of people who were too smart.”
So, doctors may have unique advantages, but they also have unique barriers. If there is a difference, is there reason to believe it’s stark enough that it wouldn’t work for other addicts?
A second group of objections center around the cost of this model. While the costs of this model will not be insignificant, it could be implemented in a manner that keeps it affordable in the context of health care spending. At current public funding rates in Michigan, the following services could be provided over 5 years for under $45,000: 120 days of residential treatment, 364 drug screens, 100 outpatient group sessions, 100 outpatient individual sessions, and 5 years of recovery support and monitoring from a Recovery Support Specialist.
In the context of American healthcare spending, this does not seem to be an unsustainable burden and, in fact, is likely to be a very wise investment in pure financial terms. According to The Healthcare Bluebook, it’s similar in cost as inserting a stent–just the procedure, excluding continuing care, medications, etc. 1,000,000 stents are implanted in the US every year.
The third set of objections focus on use of coercion. Doctors often participate in these programs under threat of having their medical license suspended or revoked. Many argue that coercion is a critical element in the success of the model and that transferring the model to other patients without the element of coercion would not get us similar outcomes because coercion is such an important ingredient. This is a compelling argument. Being a doctor is more than just a high paying job—it’s a personal identity as well as professional, and it provides a powerful source of meaning and purpose. The risk of losing their license is a very big stick, and the opportunity to return to practice is a very big carrot.
However, addiction professionals routinely encounter patients who are at risk of losing their children or their freedom. How can we be so sure that threats to their professional lives provide a unique source of motivation that cannot be created for other populations? Do we really believe that the an identity like mother or father is less powerful?
This raises two questions. First, how do we build similar systems to initiate and support recovery around these other patients? Second, how can we voluntarily engage patients into these systems of care?
Fortunately, William White has developed a model of care in response to these questions. His model of Recovery Management is recovery-oriented (rather than pathology-oriented) and is based on the assumption that addiction is a chronic illness that requires management over the lifespan. Recovery Management focuses on the following elements 5White, W. (2005). Recovery management: What if we really believed that addiction was a chronic disorder GLATTC Bulletin, September, 1-8. Chicago, IL: Great Lakes Addiction Technology Transfer Center.:
- Models of engagement that focus on lowering thresholds, outreach and pre-treatment support services, viewing motivation as an outcome of the service relationship rather than a precondition for service initiation.
- Models of assessment that are focused on the whole life of the recovering person, recovery capital, and continue over the span of the service relationship.
- Service models that recognize recovery initiation and recovery maintenance are different processes requiring different forms of support, including sustained monitoring, stage appropriate recovery education and coaching, assertive linkage to local communities of recovery, and, when needed, early reintervention.
- A shift in the locus of care from within the walls of the agency to the natural environment of the client.
- Viewing the client as the expert on their lives, goals, and, eventually, the long-term management of their recovery rather than seeing them as the biggest barrier to their own recovery.
- A shift toward service relationships as partners and allies and away from relationships that are time-limited and hierarchical.
- Models of evaluation that focus on measuring the long-term effects of multiple service interventions rather than the short-term effects of single interventions.
An important benefit of this model is that it side-steps arguments over one-size-fits-all approaches by setting our focus on providing long-term recovery management.
Many states and systems of care are attempting to deploy this model, however the implementation is often incomplete, inconsistent, too focused on individual interventions, and lack comprehension of the larger vision of the model.
Social workers are the ideal addiction professionals to execute this model. Our belief in social justice requires us to challenge the disparities in care between these culturally empowered professionals and the rest of the population. Our person-in-environment perspective and strength-based approach make us the right professionals to perform assessments and deliver services within the Recovery Management model. What group of professionals is as capable of organizing communities to support recovery and reduce stigma?
As the country struggles with the consequences of the opioid crisis and temptation builds to lower the bar by narrowing our focus to the amelioration of those consequences, social workers possess the skills, values, and conceptual frameworks to construct systems of care that deliver recovery and social justice.
References
Guest blog by Kevin Minnick, MS LMHC LCAC

Many times over the last bunch of years, I’ve run into someone who is making a recovery attempt and has a “diagnosis” of a mental health issue. Knowing full well that something like that would complicate treatment, I’ll inquire: “So tell me, what were you diagnosed with? And when was that?” To which the response goes something like this: “Well I was diagnosed with Bipolar when I was 15.” And the person is 30 years old now. Wait, what?
It goes without saying that any diagnosis carries stigma with it, whether it’s heart disease, diabetes, or any other situation that humanity will encounter. But a mental health and/or substance use disorder diagnosis is particularly difficult to shake because a diagnosis can become a label for the rest of someone’s life. So what’s someone to do when it comes to recovery?
Let’s deal with a couple scenarios that tend to repeat themselves over and over.
Remember my first person who was diagnosed in their teens and have carried the diagnosis with them since then? If you find yourself in this situation, then first and foremost, it might be a great idea to have an updated evaluation completed. The problem with having a diagnosis so early in life is this: as you grow, things will change. Mental and emotional issues are sometimes transient for young teens growing into adulthood. While you may present with a set of features that certainly look like diagnosis A when you’re 15, by the time you’re 21 everything looks different. And very often, whatever was there before isn’t there anymore. What’s this mean?
What it means is this: when you’re a teen, hormones cause more problems than a submarine with screen doors. Hormones wreak havoc on your body, your mind, and your emotions. Once you start to mature, everything seems to calm down. So a diagnosis of any type in your teens should be reevaluated once you reach adulthood (usually around 25) to see if, in fact, you really have a behavioral health issue. Better safe than sorry, my grandma used to say.
The second is where a diagnosis took place, say, several years ago and there doesn’t seem to be any improvement. “So,” says I, “who gave you the diagnosis? And what was their recommendation for treatment?” And then I hear: “I went to my family physician who prescribed me X and that was it. I’ve been on it ever since.” While the person felt better for a little bit, eventually a return to using substances became the pathway by which we ended up crossing paths. What happened?
Well, research indicates that medicine alone is not really all that effective. Talking about the situation with a trained professional that can teach you some self-management techniques shows the best promise for longer term recovery when it comes to behavioral health issues. And a follow up with a trained doctor specializing in behavioral health (mostly referred to as “the shrink”) will also be able to determine if you need more, less, or any meds at all. Things change and so should your treatment plan.
Overall, in SMART Recovery, we have tools that can be applied to many different situations. I’ve seen people with mental health issues use SMART tools to get out of situations they find difficult; we don’t have to be captives to a “label” or “diagnosis” and just think that this is as good as it gets. If you’re struggling with something beyond your recovery, get SMART and get some help from people who can guide you toward living better.
PLEASE NOTE BEFORE YOU COMMENT:
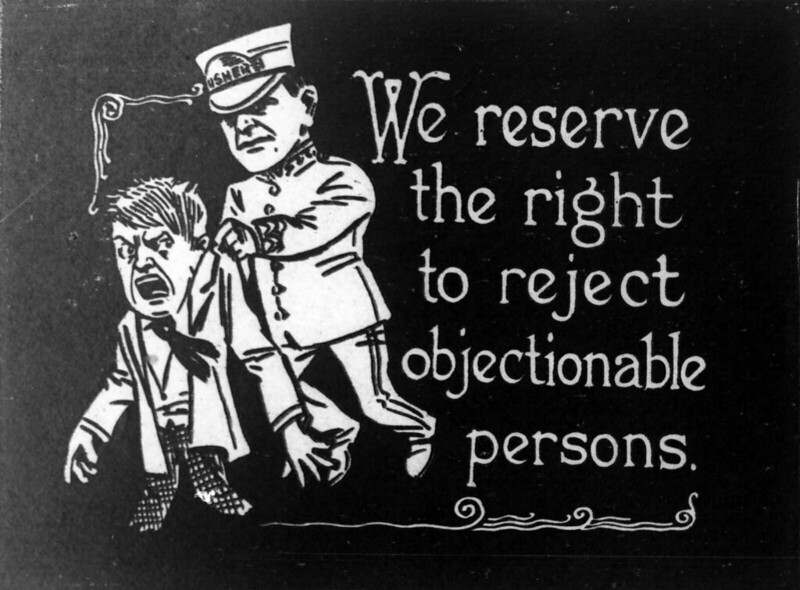
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
I recently came across a couple of items responding to reactions to research findings that were considered objectionable.
First, Noah Smith responds to calls to suppress findings that parental incarceration is correlated with the following benefits to their children, “reducing their likelihood of incarceration by 4.9 percentage points and improving their adult neighborhood quality.”
Smith has argued against mass incarceration and shares other’s concerns about how these findings may be used but pushes back against any suggestion that findings like these ought to be suppressed.
So what should scientists do? Should they become a caste of pure truth-seekers, removing themselves utterly from the world of politics and public affairs in order to pursue the facts in as objective a way as possible? Certainly not. Scientists are humans like everybody else, and they have a right — and perhaps even a duty — to try to make the world a better place through politics.
But in order to follow both the scientific ideology and their own political ideology at the same time, scientists have to manage a special sort of internal bifurcation. When seeking the facts they have to be as objective as they can, and faithfully publish what they find, but then immediately forget about that objectivity as soon as they’re doing anything other than research!
He argues that this may tie researchers up in knots, but it’s the best way to proceed.
Next, on Twitter, an addiction medicine doc and advocate responds to reactions to an unpublished paper that suggests naloxone distribution creates a moral hazard. (I posted about this a few years ago.)
He cautions against trashing the researchers on pragmatic grounds–one of them is doing work that supports progressive criminal justice agendas, that trashing from the right adversaries can actually increase her influence, and the bad optics of a bunch of men engaging in personal attacks on a woman. He also points out the frequent hypocrisy of “it’s science” arguments and, instead, asks for help picking apart the methods used in the paper.
Around the same time, I also came across this article in The New Social Worker about integrating evidence into practice. The author urges readers to consider 4 things: “what intervention/s was/were tested; who was sampled in the study; what measures were used in the study (if a quantitative study was conducted), and; what the results of the study were).”
Good advice, but that isn’t what caught my attention. After considering those 4 elements, the reader should synthesize the findings and “tell the story“ of what the studies say.
It seems to me that this is often the crux of the problem–the story we tell based on a set of findings. Despite all of the calls for us to “follow the science“, science can’t determine our priorities, values, goals, etc. We have to decide what endpoint we want to pursue and science can tell us something about how realistic it is and what pathway might be most effective at getting us there.
I’m not a scientist or researcher, but many of these arguments strike me as missing what science is capable of, particularly in the social sciences, and what we should do with science.
First, the notion that science will be free of bias strikes me as wishful thinking. Science is biased by the profession and orientation of those conducting research, by what can get funded, by what can be easily measured, by what can be accomplished in the time-frames acceptable to funders and researchers, by what can get published, by the questions that interest the researchers, etc.
Second, I tend to think that what research can tell us is fairly limited. Science, generally, cannot tell us what to do. Research can provide information that can help us decide what to do. The information it provides is often narrow and context-specific. It can’t tell us The Truth, but it sometimes can tell us a truth. Even that narrow truth is subject to review and change as new information becomes available.
Third, it’s up to us to decide our goals, priorities, what’s an acceptable outcome, what’s intolerable, how we define our context, what information is most applicable to the context we’re working within, and what story the available pieces of information tells us. For example, consider a patient who is receiving end-of-life care. Science may be able to tell us treatments that might extend her life for 6 or 12 months, but it can’t tell us whether that’s good. She and her family have to make judgments about her quality of life and priorities. Maybe her quality of life is so poor that extending her life is not desirable. Or, maybe her priority is quality time with her family, including a vacation, and the treatments to extend her life would not permit that.
Fourth, many of these arguments fail to acknowledge, value, and integrate experiential knowledge. Empirical knowledge is important, but it’s only one way of knowing and is incomplete. Borkman explained the importance of experiential knowledge this way, “As sources of truth, professional and experiential knowledge are not mutually exclusive. First, even professionals use some experiential knowledge in their practice. Newly credentialed professionals are not regarded as seasoned until they have had personal experience in the real world of work.” 1Borkman, T. (1976). Experiential Knowledge: A New Concept for the Analysis of Self-Help Groups. Social Service Review, 50, 445 – 456.
So… when we encounter findings that trouble us, how should we respond? We can question the methods and whether these findings are likely to be replicated. We can question whether it’s applicable to the contexts we work within. We can question the real-life significance of the findings. We can ask whether the researchers asked the right questions–the questions and answers that are most relevant to the people involved and the practitioners serving them.
In many cases, the objection is less about the actual data and more about the story being told with the information. For example, imagine we found no methodological problems in the study that found the 4.9% reduction in likelihood of incarceration improvements their adult neighborhood quality for children of incarcerated parents. I’d have questions about the significance of those findings and the definition of adult neighborhood quality, but let’s imagine all those questions were satisfied.
What bothers me is the support for a story that parental incarceration benefits their kids. If the information is solid, this information can, and should, provoke questions, including:
- If it’s clear that these kids experience improvements in these domains, how important are they?
- What are the other important domains that influence the present and future quality of life for these kids and their families? How are these affected by parental incarceration?
- Are these improvements evenly distributed?
- For example, do children of violent parents experience significant improvements while other kids experience adverse effects in these areas?
- What are the mechanisms of the improvements these kids experience?
- For example, is it a function of kids moving in with a stable family member?
- If the wrong story is being told, what’s a better story? Something like, “system fails to support kids until a parent is incarcerated”? (I have no idea if that’s accurate, but it’s just an example of a narrative constructed around a finding.)
Most importantly, it should provoke questions about how we might have facilitated these improvements without the incarceration of a parent. (Maybe before the incarceration and even preventing the incarceration.)
Again, I don’t know anything about the motives, methods, and rigor of this research, but some of these arguments turn into battles about who gets to produce and own knowledge. This seems especially strange in the social sciences where we are dealing with so much complexity that isolating causal factors often seems hopeless.
Instead, we might be better off using these moments to explore the story being told and the values involved. If we wish to reduce incarceration and improve the lives of at-risk kids, can we use this information and discussion as an opportunity to ask better questions, to commit to pursuing more helpful information, to clarify our values, to better live our values, to improve the lives of these kids and their parents?
These disputes come up all of the time in all sorts of areas. Unfortunately these disputes too often resemble power struggles seeking professional and ideological domination and invalidation of “adversaries”rather than the expansion of knowledge and interventions. I’ve participated in these dynamics and I regret it. Today, I try to engage troubling findings in good faith to see what I can learn and add to the discussion.

This week I ran across a wonderful STAT News article by Dr David Eddie and Dr John Kelly “People recover from addiction. They also go on to do good things,” it was published a few days ago. One of the motivators for me writing this blog article is to draw attention to it in hopes that people read it. If you do nothing else, stop here and read the linked article above. It is an exceptionally well written piece that every policymaker in the nation should consider. I clipped out this section, with intact embedded hyperlinks to draw attention to what they are saying below:
“Around 75% of people seeking recovery from a substance use problem achieve their goal, though it may take them some time to achieve full remission. The average number of attempts before success is five, though the median number is just two, meaning that a small number of outliers — usually individuals with the greatest addiction severity and other concomitant mental health issues — who need five-plus attempts, inflate the numbers, making them look worse than they are. Along with several colleagues, we recently completed a landmark study which, for the first time, comprehensively surveyed Americans who said they had resolved an alcohol or other drug problem.”
This is incredible work, and research continues to confirm what people in recovery (who are the experts on recovery) have known for a very long time. We get better, and when we do, we are assets to society. When we recover, we also save an incredible amount of resources as we are no longer costing society resources in a myriad of ways. I figured this out about a year or so into recovery, around the time I first started working in the SUD field.
I was so excited even in those days about what research was showing us. I would share the developing body of literature with anyone who crossed my path. Around 2001, we learned that treatment resulted in a 7:1 ratio of benefits to costs. I can only imagine what it would find if we factored in recovery support services in. They didn’t exist then. At the time, I figured that all we would need to do is let the world know, policies would change and we could build a robust care system. We would not just keep people alive. In recovery we thrive. We would drastically reduce the number of persons trapped in the criminal justice system and the consequences of addiction in our hospitals and human services programs.
Of course, that is not what happened. Research did not drive the conversation in the direction of expanding access to services that even averaged the minimum threshold of effectiveness or addressed drop out in any systematic way. Services remained fragmented, lengths of stay generally did not budge and may even have decreased over the years. We failed to develop and address care that followed the person until we hit the right individualized combination to meet their needs. The stats clipped above from the article are remarkable – 75% of people seeking recovery eventually achieve their goal. Can we imagine what this would look like if we systematically engaged people earlier and stuck with them until they got better with comprehensive services? It would change our society. The question is will we ever do it?
Colleagues who have been around longer than I recount to me similar experiences in the 1980s and work they did to educate the public about the benefits of helping people who have substance use issues. The impact of these efforts and the favorable research available at that time was not enough to sway the public or policymakers. We didn’t fund care or increase access, or move things towards more comprehensive services. It just didn’t happen. Fragmented, short term care for some, but not all people who need it has been the gear we have been stuck in since before the age of Disco.
There is an immense reservoir of implicit bias across society about addiction and recovery. History shows us that we do not want to help people even if saves money and lives. We expend our resources on punishment and unending devastation. Afterall, “those people” did it to themselves. We do not want to help “those people” even if it makes sense for every other reason. People in recovery play a roll too. A person wiser than I observed a lot of us recovering people pull punches and don’t speak out nearly as much as we should given the extent of the devastation and death across our community. The most fortunate of us smile and sit at the table as tokens even as nothing changes, and we bury our family and friends. In a subconscious way, perhaps we buy into the moral model believing we don’t deserve better care. Perhaps we believe we did it to ourselves and so we don’t deserve better.
I applaud Dr Kelly and his team of researchers who have made such huge contributions to what we know. They are doing invaluable work. We are in their debt. I hope society pays attention. The truth remains:
We typically get better, and when we get better, everything else improves too.
The fundamental question is whether society is ready to focus on redesigning care around long term wellness for all of our diverse communities because it makes every bit of sense to do so. I hope this time that science wins over bias. The world would be fundamentally better place in such a sea change.
Jason Schwartz guest-edits Recovery Plus Journal. Stimulating and relevant articles on: what’s essential for recovery to happen, recovery-oriented harm reduction, problems with ‘sticking with the evidence’, moral injury, and some surprises with language and stigma. Good weekend reading!

This was originally published in a recent National Association of Social Workers’ Alcohol, Tobacco and other Drug specialty section newsletter. It summarizes our addiction professions in the pandemic series.

Mike Massey has been facilitating SMART Recovery Online (SROL) meetings since 2013. His professional experience as a former teacher and union leader, as well as his personal experience with substance use, gave him the skills and abilities to help meeting participants. When many of the participants said they also were dealing with a mental health disorder, he struggled with how best to help them and decided there needed to be a reference guide for facilitators on how to handle this aspect of recovery. So, he and several others created one: Facilitator Best Practices for Addressing Mental Health Disorders and Suicide in SMART Recovery Meetings.
In this podcast, Mike talks about:
- What led to writing the Facilitator Best Practices for Addressing Mental Health Disorders and Suicide in SMART Recovery Meetings
- Most facilitators are not experts or professional therapists, but should have a familiarity with mental health disorders
- People coming to the meeting for hope and inspiration
- Reframing the terms of mental health
- Two types of stigma – self and society
- Searching for patterns and reasons for addictions
- Asking participants, “What do you need to get through this?”
- The mystery and magic of being in a meeting
- Doing a better job of helping others help themselves
- How to handle the mention of suicide
- Contributors in writing the guide, including the QPR Institute
- Finding the guide on VolunteerHQ
Additional resources:
Click here to find all of SMART Recovery’s podcasts
PLEASE NOTE BEFORE YOU COMMENT:
SMART Recovery welcomes comments on our blog posts—we enjoy hearing from you! In the interest of maintaining a respectful and safe community atmosphere, we ask that you adhere to the following guidelines when making or responding to others’ comments, regardless of your point of view. Thank you.
- Be kind in tone and intent.
- Be respectful in how you respond to opinions that are different than your own.
- Be brief and limit your comment to a maximum of 500 words.
- Be careful not to mention specific drug names.
- Be succinct in your descriptions, graphic details are not necessary.
- Be focused on the content of the blog post itself.
If you are interested in addiction recovery support, we encourage you to visit the SMART Recovery website.
IMPORTANT NOTE:
If you or someone you love is in great distress and considering self-harm, please call 911 for immediate help, or reach out to The National Suicide Prevention Hotline @ 800-273-8255, https://suicidepreventionlifeline.org/
We look forward to you joining the conversation!
*SMART Recovery reserves the right to not publish comments we consider outside our guidelines.*
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
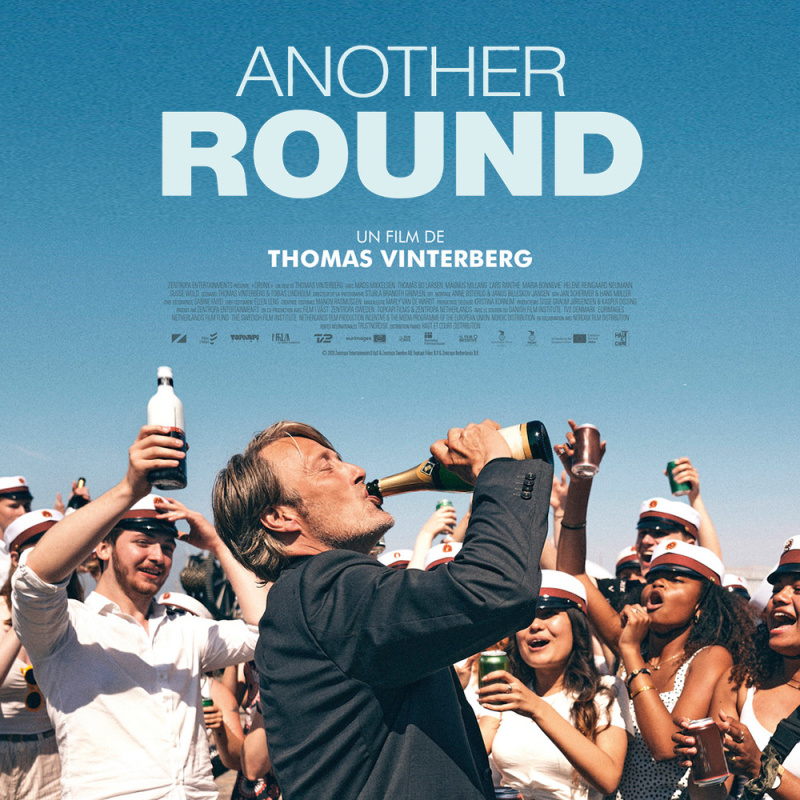 Guest blog by SMART Recovery Facilitator Ted Perkins As a veteran of the film industry who’s also a SMART Recovery meeting facilitator, I enjoy finding films that tackle the subject of alcohol abuse. I’ve rented every film there is, from dark and daring classics like LOST WEEKEND and DAYS OF WINE & ROSES, to contemporary […]
Guest blog by SMART Recovery Facilitator Ted Perkins As a veteran of the film industry who’s also a SMART Recovery meeting facilitator, I enjoy finding films that tackle the subject of alcohol abuse. I’ve rented every film there is, from dark and daring classics like LOST WEEKEND and DAYS OF WINE & ROSES, to contemporary […]
This was originally published in a 2018 National Association of Social Workers’ Alcohol, Tobacco and other Drug specialty section newsletter. Bill’s recent post on moral injury got me thinking about Sandra Bloom’s concept of moral safety, which got me thinking about this article.
Before the pandemic began, we frequently talked about the workforce moral, social, psychological, and physical safety hazards being universal and serious enough to warrant workplaces thinking about their safety obligations in the same way they are obliged to provide PPE (personal protective equipment) in hazardous situations.
It may not be as timely as it was a few years back, but it’s adjacent to Bill’s post. So… I decided to share it here.
“The expectation that we can be immersed in suffering and loss daily and not be touched by it is as unrealistic as expecting to be able to walk through water without getting wet. This sort of denial is no small matter. The way we deal with loss shapes our capacity to be present to life more than anything else. . . . . We burn out not because we don’t care but because we don’t grieve. We burn out because we’ve allowed our hearts to become so filled with loss that we have no room left to care.” (p. 52)
Rachel Naomi Remen (1996)
By now, readers of this publication may have become numb to the near daily stories about the opioid crisis. The scale and persistence of the crisis is staggering. From 1999 to 2016, the death toll climbed to 351,612 (Felter, 2018) and is continuing to accelerate rapidly. The publication STAT asked 10 public health experts to forecast the death toll for the coming decade—the average of their predictions was 500,000 deaths (Blau, 2017).
The crisis is eclipsing every other issue in addiction services. Many angles have been covered, including the scale of the overdose crisis, the role of race in the public policy response, the impact on child welfare, the suffering of bereaved mothers and their advocacy activities, the role of harm reduction, and on and on.
An important, but neglected aspect of the crisis has been its effect on the addiction workforce. What kind of toll do these deaths take on social workers and other addiction professionals? How can workers protect themselves from burnout and vicarious trauma? How can agencies protect and support their workforce?
With so little written on the subject, workers and agencies are left to find their own way to maintain professional wellness while serving people with Opioid Use Disorders (OUD), their families and their communities.
As the clinical director of a community-based addiction treatment and recovery support program, these questions became important. While we had some knowledge of burnout, vicarious trauma, and self-care, these matters became salient in new ways. This article shares some of our experiences in the face of the crisis.
Our program primarily serves people with high severity SUDs and services are organized around long-term engagement and facilitating involvement in the recovering community. It is common for us to stay engaged with clients for 18 months and many of them provide support to current clients for years and decades. We also have dozens of members of the recovering community visiting facilities every day. Historically, this had been a powerful protective factor against burnout—every day, staff see living proof every day that their work is important and effective.
As the crisis escalated, we found ourselves convening increasingly frequent sentinel event meetings (A meeting to identify the root causes of an unanticipated event involving serious injury or death.) for overdoses. Of course, we spent considerable time seeking better ways to meet the needs of our clients and prevent overdoses. At the same time, we found ourselves increasingly concerned about the effect these losses were having on our staff. We reached out to other programs to hear about what they were seeing and how they were supporting their staff. To our surprise, they were aware and concerned about overdoses as a national issue, but they were not directly affected to the degree that we have been. This led to a surprising realization—that our long-term engagement with clients, their families and our connections in the recovering community (our historical protective factors) are risk factors for burnout and vicarious trauma in this crisis. It seems we hear about every overdose, while other programs often don’t learn about overdoses that occur once patients leave their programs. Further, our deep involvement in the community means that we become a source of support for people throughout the recovering community, many of whom have never been clients. (e.g. volunteers, family members, attendees of education events, community members that support and sponsor clients, etc.)
It took some reflection to notice this and consider how to respond, and it was not always a planned, purposeful process. We eventually gravitated toward framing it as a safety issue for staff, as described by Bloom (2013). Bloom is an expert on trauma-informed care and describes a “safety culture” as an essential element of any trauma-informed system. A safety culture addresses four interacting safety domains: physical, psychological, social and moral (2010) Attention of parallel process is also critical, as systems in sustained close contact tend to develop similar patterns of thoughts, feelings and behaviors (2012). This means it is not possible to maintain a safety culture for clients without also maintaining a safety culture for staff.
Moral safety is probably the least concrete of these domains but it was one of the first domains on our radar. We were concerned about the moral distress that staff might be experiencing, including:
- a gnawing sense that they’ve failed their clients, client’s families, colleagues, community and organization;
- a vague sense that they could have and should have done more;
- wondering if we were living up to our organizational and personal values;
- ideas about what could be done to prevent overdose, but a sense that their supervisor or organization won’t seriously consider it; or
- a sense (real or imagined) that interrogation of our practices would not be accepted.
We sought to ensure moral safety by making a concerted effort to ensure open dialogue in sentinel event meetings. We developed a preamble to the meetings, stating and restating that the purpose of the meeting was to learn and improve, not to assign blame. We also tried to convey a desire to discuss anything that seemed relevant to anyone at the table—that nothing is taboo. Administration took the lead by asking challenging questions about agency policy and whether the problems we face demand new practices and an evolution in organizational philosophy.
It didn’t take long for social and psychological safety issues to emerge. Many of these questions were unspoken, but just beneath the surface:
- I’m a professional, should I be feeling this grief?
- What if I cry? How will others respond? What will they think of me?
- I want to reach out to the family. Is that about my needs, or theirs? If I share that thought, will others see that as a boundary problem?
- I’m angry at the client. If I share that feeling, will others judge me?
- I’m noticing some things I think I failed to do. What will others think? Will they blame me?
- I don’t know if I can keep doing this work. Will others think I’m weak or not committed?
- Do I know what I’m doing? Do we know what we’re doing?
We addressed these safety issues by expanding the sentinel event preamble to create an expectation of grief and inviting everyone to share their thoughts and feelings as addiction professionals and as human beings who have experienced a loss. It also reminds us that this experience of loss is not a problem to be solved. As such, our response will be to listen generously and care for each other, rather than attempt to fix it.
Again, it was important that organizational leaders modeled sharing their thoughts and feelings, even if it made them feel vulnerable. This made it possible for others to do the same. Many of us imagined that this might open floodgates and consume considerable time and resources. This has not been the case. It appears the most important element is creating space for staff to share their reactions and support each other. The result is actually the opposite of what we feared. Staff spend less time ruminating, they are less anxious, and are more connected to each other in ways that support each other’s wellness and growth.
This has not just been about protecting the wellbeing of our staff. As a result, we’ve been able to work together to adapt policies, develop new practices and improve existing practices to prevent overdoses, improve recovery monitoring and follow-up, improve collaboration with other providers, improve informed-consent, and identify and provide support for others affected by the overdose.
We don’t profess to have all the answers and are very interested in hearing how other agencies are weathering this crisis. Please consider sharing your experience below, if we get enough responses, we’ll publish a follow-up.
References
Blau M. (2017). STAT forecast: Opioids could kill nearly 500,000 in U.S. in next decade. STAT. Retrieved 11 June 2018, from https://www.statnews.com/2017/06/27/opioid-deaths-forecast/
Bloom, S. L. (2010). Organizational Stress as a Barrier to Trauma‐Informed Service Delivery. In Becker, M. and Levin, B. A Public Health Perspective of Women’s Mental Health, New York: Springer (pp.295‐311).
Bloom, S. L. (2012) Building Resilient Workers and Organization: The Sanctuary Model of Organisational Change. In N. Tehrani (Ed.), Workplace Bullying: Symptoms and Solutions (pp. 260-277). London: Routledge.
Bloom, S. L., & Farragher, B. J. (2013). Restoring sanctuary: A new operating system for trauma-informed systems of care. Oxford: Oxford University Press.
Felter C. (2018). The U.S. Opioid Epidemic. Council on Foreign Relations. Retrieved 11 June 2018, from https://www.cfr.org/backgrounder/us-opioid-epidemic
Remen, R. N. (1996). Kitchen table wisdom: Stories that heal. New York: Riverhead Books.
Helping Others, Why Sponsoring is Important to Recovery
Step 12 of Alcoholics Anonymous says:
“Having had a spiritual awakening as the result of these steps, we tried to carry this message to alcoholics, and to practice these principles in all our affairs.”
At its core, this step reminds you to live your life by the principles of AA, and to also encourage others like you in need to discover the promises of the program. As you go through your recovery journey and work the steps, you will build the foundation for your life in sobriety.
However, you probably didn’t get to Step 12 by yourself. No, many individuals in the rooms of Alcoholics Anonymous and/or Narcotics Anonymous probably helped you along your way. From sponsors, to home groups, to just plain peers and friends, the fellowship found in 12-Step Programs is focused on learning for oneself and going on to give back. As you have improved your life greatly, it is important that you help others who are suffering.
It can also be beneficial to your long-term sobriety and recovery. Here are some ways giving back and helping others can support your recovery:
Builds Self-Esteem
To put it simply, giving back never feels bad. To have the opportunity to listen to others and to genuinely relate to their strife like no one else can is a beautiful thing. Throughout your time in recovery, you have made mistakes, and you probably had to seek the counsel and wisdom of others to overcome obstacles or to bounce back when you’ve taken a wrong turn. As you learned, you built on your experience and knowledge along the way. Passing this on to someone else can instill a sense of leadership and mentorship within you, and can build your confidence in your own ability while helping someone else simultaneously.
Fills Idle Time
An enemy to those in recovery can often be boredom or idle time. No matter how far you are along in your recovery, boredom can lead to those familiar feelings of loneliness, isolation, and depression from days of active use. Helping others by way of volunteering with or sponsoring other individuals in recovery fills up your time and gives you new connections to grab coffee with, go to meetings with, or plan other events with to keep your schedule full.
Can Prevent Return to Use
When cravings or thoughts about returning to use present themselves, it can be difficult to think clearly. You might find yourself glamourizing your past at times, struggling to remember why active use was so detrimental to your life.
Serving and helping others who are suffering may serve as a reminder to yourself when you were in the throes of the earliest parts of your sobriety and recovery, further reinforcing the importance of your dedication to a 12-Step Program and to your own sobriety.
Gives You a Sense of Purpose
Finally, helping others can give you a sense of purpose. Knowing that someone else might lean on you for support in their journey to stay well can make you feel a sense of accountability, a reason to get out of bed in the morning when that reason can be difficult to find or feel.
Helping someone else can make you feel needed, it can make you feel important…because you are.
Remember, helping others doesn’t have a requirement. Just showing up, living your life by the 12 Steps, being honest and open, and meeting all of those around you with love are the greatest acts of helping others that you could possibly participate in.
***
For more information, resources, and encouragement, “like” the Fellowship Hall Facebook page and follow us on Instagram at @FellowshipHallNC.
About Fellowship Hall
Fellowship Hall is a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.

