In this essay I make two claims. My two claims will take the form of slightly changed versions of two borrowed sentences. (I will present the original versions of the two borrowed sentences later in the essay). I simply took the borrowed sentences and changed a few key words. In my changed version of each sentence, you will see in italics the words I inserted to replace certain words found in the original sentences.
Here are my two claims:
- For recovery advocacy, no consistent system of axioms whose theorems can be listed is capable of proving all truths about recovery.
- There will always be statements about natural recovery that are true but that are unprovable within the system. And recovery cannot demonstrate its own consistency.
By extension, then, I state that recovery itself is, in a manner of speaking, “false”, or “unprovable” – but useful anyway.
What is interesting is that the program of 12-step recovery is a total system, not just an “outcome”.
(By “total system” I mean to highlight at least two things. First, the 12-step version of recovery concerns the whole matter of one’s alignment to one’s self, others, and the world at levels including behavior, thoughts, values, priorities, and personal development over time. Secondly, not only is 12-step recovery focused on a wide scope of personal change, but it also provides and encourages development of a social structure within which one can undertake and live out the work itself, and one’s recovery.)
Criticism from Empiricism
Critics of traditional 12-step recovery criticize it on various grounds. Critics often assert that the most compelling arguments against it are those we find under simple scientific scrutiny.
That criticism is traditional. For thousands of years in the west, tools of verification have included formal logic, math, and structured observation. Later, the scientific method as we know it arose.
As a process, empiricism clears the air of superstition and false beliefs. Periodically, applying processes of logic, observation, or scientific study exposes some “facts” (that have long functioned as “received knowledge”) as actually nothing more or less than simply false. Examples include setting aside the notion of a flat earth, a solar system with the earth at the center, and so on.
On the tree of science1, the study of social systems is held to be the most spongy and most lacking of rigor. Or so it is claimed. After all, the real science inside the study of social groups is psychology. And of course, for psychology the more pure real science is biology. If one knows everything about biology, one will already have psychology. And for biology we all know the real science is chemistry. But chemistry is nothing more than applied physics; learn physics and you will have the essence of chemistry. Last and best of all is math itself – the pure content that is the essence of physics and core material of the scientific method. Math is most pure. Or so it is claimed.
For thousands of years in western philosophy it has been set forth that everything that is true: 1) must not be self-contradictory or internally inconsistent and 2) must be provable and subject to proof.
Certainly, math is best and most pure of all.
Math Is Not the Path
But interestingly, math itself is nothing but a model and under proper scrutiny math collapses in violation of itself and of our hopes. The quotation that follows expounds that fact and lists as numbers 1 and 2 (I added the numbers themselves for clarity) the two borrowed sentences I used to start this essay.
“Gödel’s incompleteness theorems are two theorems of mathematical logic that demonstrate the inherent limitations of every formal axiomatic system capable of modelling basic arithmetic. These results, published by Kurt Gödel in 1931, are important both in mathematical logic and in the philosophy of mathematics. The theorems are widely, but not universally, interpreted as showing that Hilbert’s program to find a complete and consistent set of axioms for all mathematics is impossible.
The first incompleteness theorem states that no consistent system of axioms whose theorems can be listed by an effective procedure (i.e., an algorithm) is capable of proving all truths about the arithmetic of natural numbers.
- For any such consistent formal system, there will always be statements about natural numbers that are true, but that are unprovable within the system.
- The second incompleteness theorem, an extension of the first, shows that the system cannot demonstrate its own consistency.”2
Math collapses as a coherent system under the scrutiny of logic? Is that not a paradox? I thought the presence of a paradox, as 12-step recovery is well known for, was evidence of either illogical statements or false beliefs.
Return to Recovery
Why denigrate either “recovery” or the working a personal 12-step program based on them not being empirically valid? Besides, are there not “other ways of knowing?” And do we not see even math as a system is itself unprovable and incomplete?
The criticism of recovery and of a personal program in the rooms of 12-step recovery on the grounds of math are both in that sense false and, on arrival, in fact – dead – as statements.
A Unified and Inconsistent Model That Works
But rather than study various possible models of recovery, and compare how they compete on mathematical or empirical grounds, can we not turn the lens of observation onto the individual phenomenology of personal recovery?
Doing so would provide (like math itself) a unified and inconsistent model that works, imperfectly accommodating everything that is, including:
- Recovery-oriented harm reduction3
- Serial recovery where use of some substances has ended and use of others has not yet4,5
- Recovery from one substance (like alcohol) while addiction to another (like cigarettes) continues5
- Recovery during medication maintenance6
- Recovery starting even at the peak of severity of illness7
- Abstinence-oriented lifelong 12-step program recovery8
- Recovery continuing after dropping out of support9,10,11
- Being in recovery when you say you’re in recovery
A Final Question
Why criticize individuals and individual differences using incoherent models like math to do so, when our whole system is necessarily inconsistent?
Is it not the case that “one must cultivate one’s own garden?”12,13
References
3Recovery-oriented harm reduction
4White, W., & Kurtz, E. (2006). The Varieties of Recovery Experience. International Journal of Self Help and Self Care. 3(1-2), 21-61.
5Recovery definition – conceptual boundaries
7Jellinek, E.M. (1952). Phases of Alcohol Addiction. Quarterly Journal of Studies on Alcohol. 13(4): 673–684.
8 Narcotics Anonymous (2012). Living Clean: The Journey Continues. Narcotics Anonymous World Services, Inc.
10Disengaged styles of recovery
11Kelly, J. F., Bergman, B., Hoeppner, B. B., Vilsaint, C., & White, W. L. (2017). Prevalence and Pathways of Recovery from Drug and Alcohol Problems in the United States Population: Implications for practice, research, and policy. Drug and Alcohol Dependence, 181, 162–169.
12Condide
13Why Voltaire Said: You Must Cultivate Your Own Garden
Acknowledgment
The author thanks Jason Schwartz for comments on a previous version of this writing.
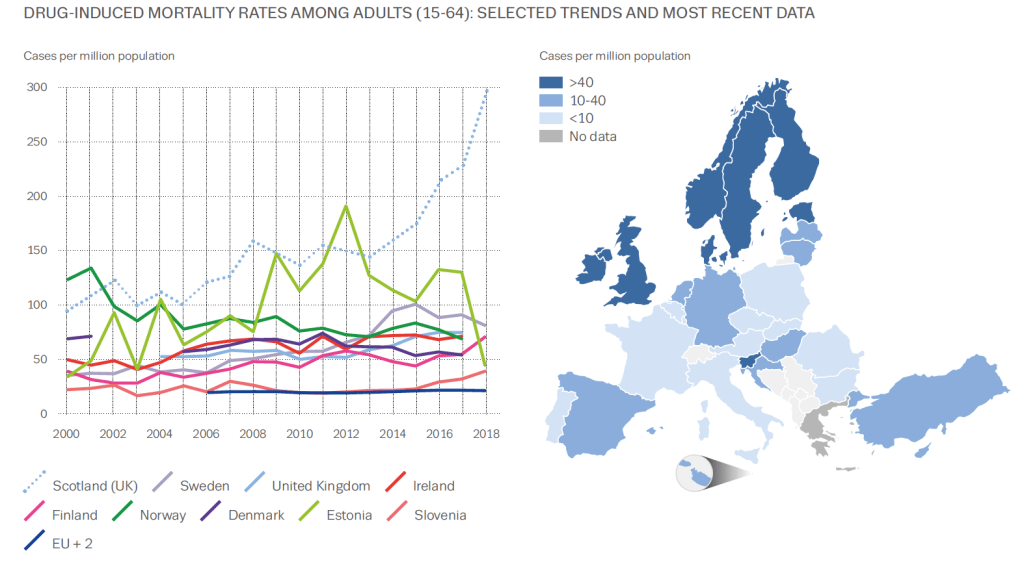 Graphic from European Drug Report 2020: Trends and Developments
Graphic from European Drug Report 2020: Trends and Developments
It’s not often graphs elicit an emotional response, but this one did for me. It’s from the EMCDDA’s recent report on drugs in Europe. The map shows that the UK has high levels of drug-induced mortality compared to most of Europe. But look at the dotted blue line on the graph. That’s Scotland. Worst in Europe and possibly the world.
It’s not a new phenomenon, our high drug-related deaths. The Scottish Drugs Forum makes the point: ‘Drug overdose deaths are preventable. We know how to prevent these deaths and yet they still happen.’
Kindness Compassion and Hope
So what’s being done about it? One of the highest-hit cities is Dundee. A commission set up to look at drug-related deaths took evidence from over 1000 people and made recommendations which included changing the system and culture, having holistic and integrated care and addressing the root causes of drug problems. The report title was Kindness, Compassion and Hope, which feels inspiring.
The Scottish Government has invested in treatment services with a particular emphasis on reaching more at-risk people and retaining them in treatment. Last summer it set up the Drugs Death Task Force, a group chaired by Dr Catriona Mathieson which has highlighted the need for wide distribution of naloxone, an immediate response pathway on non-fatal overdoses, medication assisted treatment (MAT), the targeting of those most at risk, public health surveillance and provision of equity of support for those in the criminal justice system. The Scottish Government has put £1M into research and £4M towards the task force’s six recommendations.
Standards for MAT have been developed, the country has a three week target from referral to treatment, ready access to prescribing, treatment free at the point of delivery, routine overdose prevention training, widespread naloxone distribution, generally accessible injecting equipment provision, low threshold clinics in many places and a high public awareness of the problem. In addition, there is investment in research which looks to find solutions to the problem. But is it enough? – the causes of our drug deaths are complex and rooted in poverty, exclusion, trauma and hopelessness.
A public health emergency
“What we are facing in Scotland is a public health emergency,” Joe Fitzpatrick, Scotland’s Public Health minister stated recently. “I am prepared to consider any course of action that is evidence based to save lives, whether its controversial or unpopular.”
Too controversial for the UK government are drug consumption rooms which Glasgow in particular wants to trial. Drugs policy is not devolved to the Scottish Government and Westminster won’t consider changing the law to allow this to happen, though one crusader is flouting the rules to deliver this currently.
One area in Scotland where consensus is growing is around the likely benefits of shifting to a public health approach. A cross-party parliamentary group, The Scottish Affairs Committee, held an enquiry into the subject and reported at the end of last year. It asked the UK government to declare a public health emergency making the point that the criminal justice approach has failed. It highlighted how current legislation on drugs stands in the way of tackling the issue from a public health slant.
And the UK government’s response? Pete Wishart, the group’s chair described this as ‘the almost wholesale rejection of recommendations.’ The Guardian has suggested this rejection of what multiple experts think is best for Scotland can only fuel calls for independence. When you consider that the UK government hosted a summit in Glasgow last February without consulting the Scottish Government or asking people with lived experience to attend, you begin to grasp the depth of the gulf that separates the two approaches.
The role of visible recovery
I wonder in all of this what the role is for recovering people, recovery communities and the powerful protective effects of developing strong social networks for those most at risk. What if we studied whether developing new social networks had a significant effect on Scottish drug deaths? What if we developed drug consumption rooms which were strongly recovery-orientated with visible recovery present? I suspect, that at the very least, this would boost hope. Hope is often in short supply in addiction, and anything that augments it is welcome.
Perhaps if every outreach service, every injecting equipment outlet and every treatment setting had people with lived experience prioritising the connection of those at most risk not just into treatment but also into a variety of supportive recovery-oriented settings, there could be a positive impact on drug deaths. Perhaps this would help people begin a cultural journey, moving from the culture of addiction to a culture of recovery as Bill White sets out. Not the only thing to be done certainly, our approaches need to be multiple, but something that doesn’t require the permission of the UK Government and which may augment the other interventions.
The Drug Deaths statistics for Scotland for 2019 have been delayed due to COVID, but will be published soon. I’d like to see that dotted blue line on the graph reducing, but that is by no means certain and much remains to be done.
Does mutual aid work? If you are a member of a mutual aid group that you believe is keeping you sober or drug-free, then it’s pretty much assured you will say ‘yes’. That’s understandably not good enough for researchers and some others. Nearly two decades ago, I asked a consultant addiction psychiatrist why he didn’t recommend mutual aid to his patients. ‘There’s not a shred of evidence that it makes a difference’, was his response. It’s a response I still hear fairly frequently. Actually, there was more than a shred of evidence even back then, but it was not at the level of ‘gold standard’ evidence.
Cochrane is a British-based charitable foundation which scrutinises international evidence on health interventions to help stakeholders make informed choices about what is effective and what is not. When Cochrane last looked – in 2006 – at whether there was evidence of efficacy for Alcoholics Anonymous (AA), the findings were disappointing. It wasn’t that there was evidence it didn’t work, but that there really wasn’t much quality evidence about – they could only find 8 studies worth looking at. That review has oft been quoted as ‘proof’ that AA doesn’t work.
All that has changed in Cochrane’s most recent review of the evidence headed up by John F Kelly, Keith Humphreys and Marica Ferri. There are now 27 studies involving over 10,000 people which meet the strict criteria for analysis. The large document capturing the evidence and what it means has just been published.
Kelly, Humphreys and Ferri looked at randomised controlled trials (RCTs), quasi-RCTs and non-randomised studies that compared AA or Twelve-step Facilitation (AA/TSF) with other interventions, such as motivational enhancement therapy (MET) or cognitive behavioural therapy (CBT), variations in TSF, or no treatment at all. (Twelve-step facilitation is designed to increase AA participation). The reviewers also looked at healthcare costs. Those participants in the studies were patients with alcohol use disorder who were there voluntarily.
They wanted to see if AA membership was associated with abstinence, reduced drinking days and reduced healthcare costs. There were some caveats to some of the studies which cover potential selection bias and poorer quality methods, but overall the evidence was sound.
There is a wealth of findings and I recommend reading the review or at least a summary, but I’m going to pick out a couple of the headlines.
AA/TSF when it is manualised (using specific guidance in delivering it) is better than other interventions (including CBT) at helping those with alcohol use disorder reach continuous abstinence. Not just at one year, but at two and three years after the intervention.
AA/TSF when it’s not manualised is as good as other interventions and there is evidence that it saves health care costs compared to other interventions.
That’s pretty impressive.
The authors say:
There is high quality evidence that clinically-delivered TSF interventions designed to increase AA participation usually lead to better outcomes over the subsequent months to years in terms of producing higher rates of continuous abstinence. This effect is achieved largely by fostering increased AA participation beyond the end of the TSF intervention. AA/TSF will probably produce substantial healthcare cost savings while simultaneously improving alcohol abstinence.
So what does it mean for practice? The authors say:
A relatively brief clinical intervention (AA/TSF) can help people with AUD to become engaged in a long-term, freely available, community-based, recovery support resource that can help them sustain ongoing remission. If people with AUD are opposed to attending AA, despite the strong evidence for its potential to aid recovery, clinicians might consider linkage to alternative mutual-help organisations as they may confer benefits at similar levels of engagement.
John Kelly quoted in the New York Times said:
These results demonstrate A.A.’s effectiveness in helping people not only initiate but sustain abstinence and remission over the long term. The fact that A.A. is free and so widely available is also good news. It’s the closest thing in public health we have to a free lunch.
Keith Humphreys said:
For people already in treatment, if they add A.A. to it, their outcomes are superior than those who just get treatment without A.A.
And how does it work? Kelly, quoted in Medscape News said:
The camaraderie inherent in AA and the lived experience of active addiction and recovery can reduce stigma effects — feelings of shame and guilt. The supervision and accountability that an AA sponsor (mentor) can provide has been shown to be very helpful in maintaining sobriety.
“Rigorous studies” have demonstrated AA reduces relapse risk by “helping individuals change their social networks” and “engage in a lifestyle more suited to continuous sobriety.”
It seems the standard and oft-seen negative response as to whether Alcoholics Anonymous works will now need to change, though of course it will only work if addiction professionals and others actively link their clients and patients into AA.

This is a version of a blog I published a few years ago, but thought it still relevant today.
Doug Sellman is a professor of psychiatry and addiction medicine in New Zealand. In 2010 in the journal Addiction, he attempted the difficult task of distilling the ten things you need to know about addiction from the research of the last thirty years. No mean feat.
Well, what are they?
1. Addiction is fundamentally about compulsive behaviour. In normal behaviours, the control in our brains is top down. In addiction the cortex (the decision making bit of the brain) becomes ‘eroded’ to a ‘dehumanised’ compulsion. Sellman outlines the well-studied brain circuits involved, and points out how this view creates one of the defining marks of addiction: continuing to use despite negative consequences.
2. Compulsive drug seeking starts outside conscious thought. The debate about free will (and as the prof says ‘free won’t’) gets complicated here. Apparently the conscious part of our brain is about a half second behind imprinted learned behaviours. The lag and its effects are exaggerated in addiction and well learned patterns including cues call the shots over the ‘higher’ brain’s ability to avoid damaging choices. Result: illogical self-harming behaviours continue.
3. Addiction is about 50% inherited, but it’s much more complicated. Genetic and population studies show a strong genetic element for addiction with some folk being more vulnerable than others. It gets complicated because it’s not just about a single gene or even a few, but possibly hundreds, and even then they interact with infinite variations in environment. This is not about ‘nature versus nurture’, but represents a ‘new interactive model of nature via nurture’.
4. Most people with addictions who come for help have other psychiatric problems as well. For those wanting to move away from the medically dominated model of treatment, this is a big obstacle. 75-90% of those asking for help from services have diagnosable mental health problems including depression, social phobia and post traumatic stress disorder. Alarmingly though, many of our big treatment studies have excluded people suffering from mental health problems. For those of us involved in providing help for those wanting to recover, we will need to ensure that mental health needs are not overlooked. On a personal note though: I do hold a hopefully healthy observation that many of the psychiatric labels we pick up as active addicts melt away in recovery without the need for psychiatric treatment.
5. Addiction is a chronic relapsing disorder in the majority. This was the most challenging of the ten findings for me to simply accept. Prof Sellman says that fewer than 10% of those going through treatment will experience continuous long-term abstinent recovery. He does point out that life will be better for many after treatment and that we need to accept relapse as part of the deal for many. Not doing so will prevent folk coming back for help. There is a tension in this for me between instilling hope and optimism and being unrealistically positive. Other research gives more hope for longer term outcomes suggesting more than half will achieve remission.
[Part 2 is here.]

Addiction is normally framed as a chronically relapsing disorder, but a recent research paper from John Kelly and colleagues challenges us to think again. We actually don’t know as much as we might about recovery trajectories and, in terms of the number of attempts needed, there may be grounds for greater hope.
Previous research
Kelly and his colleagues point to groundwork done by other researchers which fits in with the chronic relapsing description. More than 50% of those starting addiction treatment in the USA do not complete it, 58% have had at least one previous treatment episode and more than 50% of those leaving treatment for alcohol or other drug problems relapse within 90 days.
Smoking cessation attempts have been much better studied – the number of quit attempts before successfully stopping long term is reported to be between 6 and 30 depending on the research method. Kelly and his colleagues point out that it would be good know the equivalent number of recovery attempts for alcohol and other drugs. If it takes 30 attempts to get into stable recovery, that could well act as a disincentive to trying.
Previous research has been limited because it’s pretty much focused on treatment populations. A 2005 study by Dennis and colleagues following up 1,200 patients going through publicly funded treatment found that for those achieving a year or more of abstinence, the median time from first use to last use was 27 years and from first treatment episode to last use was nine years. Feels a bit gloomy.
This research
Kelly and colleagues set out to pin down how many recovery attempts people have on average before successfully resolving an alcohol or other drug problem. They also wanted to identify the things that predicted the number of attempts and look at the relationship between the number of attempts and quality of life in recovery.
They identified 2000 people from a survey database who identified as having resolved an alcohol or other drug problem and asked them how many prior serious recovery attempts they had made. The answers were illuminating.
One of the main findings was how skewed the data were. Attempts could be as low as one or as high as one hundred. It looks like a relatively small group of people had very high numbers of attempts which means that the average number of attempts identified (5.35) is misleading. The median (bang in the middle) number was 2. The modal (most common) number of serious recovery attempts was 1.
There was no association between number of recovery attempts and age, sex, education, or household income. Those who had been diagnosed with depressive or anxiety disorders or who had received treatment or recovery support services including inpatient, outpatient mutual help, or any support service, reported a greater number of recovery attempts.
The researchers suggest that a higher number of recovery attempts needed before alcohol and other drug problems are resolved is ‘independently related to greater psychological distress, but not other indices (e.g., quality of life, happiness; self-esteem), regardless of how long one has been in recovery, prior service use, or the presence of other psychiatric comorbidity.’
The authors theorise that there could be a group of individuals who have ‘suffered from either a greater burden of or sensitivity to stress.’ This group could have found that recovery-related changes were more challenging or ‘perhaps represents those who have found a way to stay in recovery despite a greater burden of sensitivity to stress.’
For most people, the number of serious recovery attempts needed is actually quite low, but with certain subgroups (i.e., likely those with higher severity/ chronicity/comorbidity and lower recovery capital), requiring more attempts to achieve success. Yet, it is these more severe subgroups that are perceived as the norm, when the opposite is in fact true.
The authors point out some limitations in their methodology – the cross sectional nature, the reliance on self-reporting and the non-specific term ‘serious attempts’.
What does it mean?
It’s clear that those who identify as having resolved their problems with alcohol and other drugs are a diverse group – some not having to go to treatment or access mutual aid at all, some managing to resolve their problems with few attempts and some having to have multiple attempts.
Targeting our highest intensity interventions (e.g. structured psychological therapies or residential rehabilitation) to the most vulnerable may short circuit the number of attempts needed and help them achieve their goals faster. For this we need a staged series of treatment interventions that are highly individualised (as the authors point out) and that are joined up – a recovery-oriented system of care in other words. And resources to deliver this.
Here’s the authors’ hopeful bottom line:
The median number of recovery attempts, however, was surprisingly low and may offer hope to those struggling with alcohol and other drug problems.
How Many Recovery Attempts Does it Take to Successfully Resolve an Alcohol or Drug Problem? Estimates and Correlates From a National Study of Recovering U.S. Adults John F. Kelly, Martha Claire Greene, Brandon G. Bergman, William L. White, Bettina B. HoeppnerAlcohol Clin Exp Res. 2019 Jul; 43(7): 1533–1544. Published online 2019 May 15. doi: 10.1111/acer.14067
Photo credit: istockphoto.com/lovethewind (under licence)

Nick Goodwin was a Marine Corps Infantry Officer with an attitude of invincibility. Then he ran into a wall of self-doubt. One question kept coming up, morning after morning.
“On the one hand I’m telling myself I’m the strongest person alive—you’re a Marine Corps Infantry Officer, you’ve led 300 people—and then the other part of it is saying what the heck, why do I wake up in the morning convinced that I’m never going to drink again and by 7 p.m. I’m drinking again?!”
Nick decided that the reason was a combination of factors. Here’s the short version.
Nick joined the Marines two days after his high school graduation, then spent almost nine years staying in top shape, travelling throughout the Pacific theater, becoming an officer, and being responsible for hundreds of men and women serving their country. Important, high stakes stuff. He speaks of valuable lifetime experiences in the military, including the chance to see so many different countries and shape lives. Plus, some of the fun to be had by hanging out with Australian Commandos.
Near the end of his service, the last year or so, Nick started struggling with over-indulgence of alcohol. He now sees the slide as a reaction to his pending discharge. Nick knew, without a doubt, that life was going to change dramatically, and knowledge that revved up his anxiety, which led to more drinking, which caused its own anxiety. Around and around he went, like many others struggling with alcohol addiction. But in Nick’s case, the party was just getting darker.
Upon leaving the service, Nick’s marriage fell apart. Divorce is rarely easy, and in this case, it was quite harsh. All the issues of finance, custody, living arrangements, etc. packed a punch. What made it a knockout, Nick later reflected, was the complete loss of a goal orientation for his life, something he has always had in the military.
Nick was in trouble and he knew it. He tried AA and SMART, but didn’t stick with either. He kept drinking. The rest of the details don’t really matter. What matters is what happened next.
Isolated and disconnected from others during COVID, Nick turned to the Veteran’s Addiction Recovery Center and asked for help. He wanted inpatient treatment, believing it was the only way he would succeed in what had so far been a losing battle. The VA informed him that it was not an option but suggested he try SMART Recovery again, this time online. Nick dove in and found the tools and resources he needed. The best part is that they were right for him—a hard driving, goal oriented, cocky ex-Marine with a nagging sense of self-doubt. Nick explains the connection.
“I don’t like being told what to do, which is [what you get] in a lot of the programs I found. It’s kind of somewhat of a method they use. But SMART Recovery, they view it as a choice.”
Nick believes this focus on choice is consistent with addiction itself, in that his addiction was self-managed, so his recovery should be too. He also appreciates that meeting facilitators don’t control meetings. Instead, participants share ideas and experiences with one another and use SMART materials that are practical and science-based. Whatever the substance or activity that a person struggles with, Nick explains, changing negative thinking is one of the keys.
“When they talk about leading a balanced life, to me, if you do that, addiction becomes a kind of a symptom. It has been very effective in my life dealing with depression and anxiety…without this program I wouldn’t have cured those things.”
Nick decided that he wanted to use what he knew about his own recovery as a way of serving others, so he became a trained SMART facilitator. Naturally, he directed his attention toward what he knew best helping to guide and provide opportunities for veterans. With the help of another SMART facilitator who was also ex-military, a meeting for Veterans and First Responders was started. Bringing the circle around again, this time in a positive direction.
Today, the combination of positive self-talk and a renewed goal orientation has brought Nick to a good place. The kind of place that includes purpose.
“[SMART] not only keeps me sober but keeps me enjoying life. SMART Recovery, really helping people recover, is my purpose now.”
There is a strong ripple effect when a person embraces SMART Recovery. Nick relies on SMART’s tools for himself and has chosen to pay it forward by becoming a SMART facilitator and working with veterans and First Responders. This ripple is possible because mutual support group meetings and science-based materials are available to those who desire a self-empowered, stigma-free Life Beyond Addiction, where meaning, purpose, and positive growth are the norm.
Your year-end gift to SMART Recovery will be used to launch our important work in the best possible way. Our goal is to make 2021 a less isolated and difficult year for individuals and families that are battling addictions. SMART Recovery is poised to make a significant impact and help individuals live fulfilling and meaningful lives.
Additional resources:
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
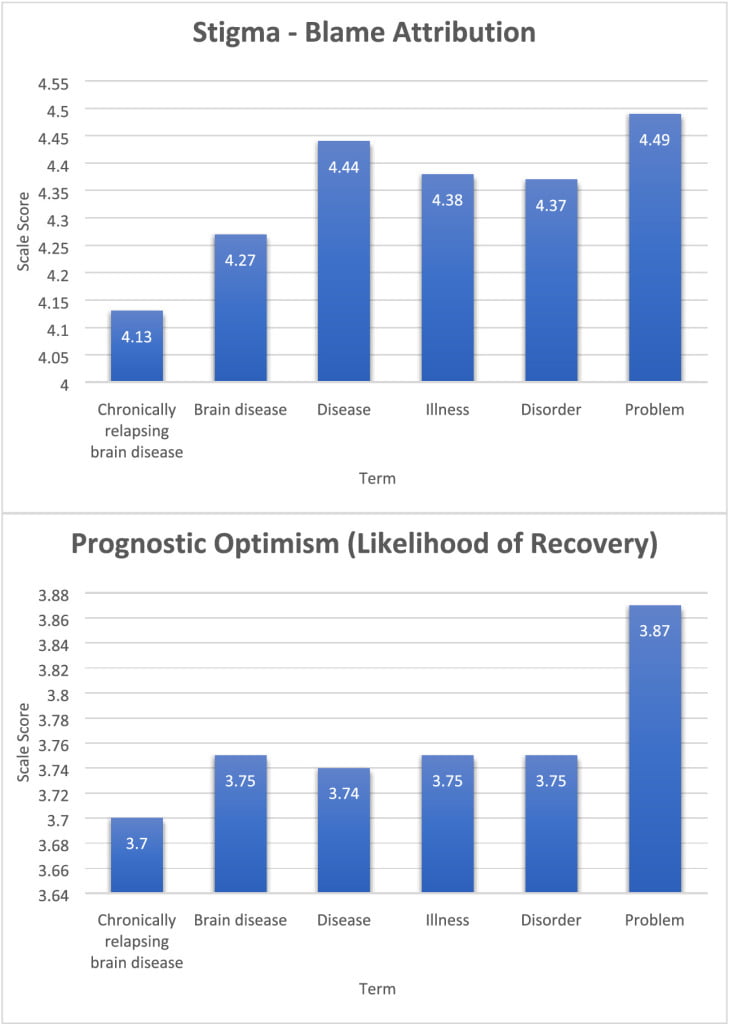
What’s more harmful? Blame or pessimism?
Kelly et al. find that ‘chronically relapsing brain disease‘ was associated less stigmatizing blame and more pessimism about their capacity to recover, while ‘problem‘ was associated with more stigmatizing blame and more optimism for their capacity to recover.
…exposure to the ‘chronically relapsing brain disease’ term was associated with the lowest levels of stigmatizing blame attributions; in fact, exposure to any other term was associated with a significant increase in stigmatizing blame although, intriguingly, the blame effect was related in a linear ordinal fashion with ‘problem’, resulting in the greatest stigmatizing blame attribution. In contrast, study participants who were exposed to the person described as having an opioid ‘problem’ compared to ‘chronically relapsing brain disease’ exhibited the strongest beliefs that the person could recover (Fig. 1), were less dangerous and less likely to require continuing care. These findings support the use of the ‘chronically relapsing brain disease’ term to reduce stigmatizing blame, but simultaneously suggest that this may not be the best term to use to convey the more positive notion that someone with opioid‐related impairment is approachable and can recover; in that case, the less medical and more generic, ‘problem’ term may be optimal.
Kelly, J. F., Greene, M. C., and Abry, A. (2020) A US national randomized study to guide how best to reduce stigma when describing drug‐related impairment in practice and policy. Addiction, https://doi.org/10.1111/add.15333.
It seems noteworthy that the currently favored term, disorder, didn’t fare well. For me, this illustrates the tail-chasing we inflict on ourselves when we let the attitudes of others determine what language is acceptable or unacceptable. We shouldn’t surprised that their attitudes are irrational and inconsistent. Can we yoke our language to their attitudes without tying ourselves in knots and surrendering a little of our agency? I’m skeptical.
We do this with hopes of benefits like greater acceptance and reduced stigma, and there’s reason to believe those benefits can be real in some situations.
Are there also consequences to this approach? I don’t know.
Could this attention to changing our language distract us from the real problem (other people’s attitudes and the real world manifestations of those attitudes)? Could it divide us because we start policing/managing each other in an attempt to reduce the negative attitudes of others? Could it create new stratifications within our communities?

Shawn Fisk is an addiction treatment counselor in Ottawa, Ontario, Canada. His lived personal and professional experiences have led him to challenge cognitive discrepancies and chart a new path for his and his clients’ lives.
In this podcast, Shawn talks about:
- The privilege of working at Serenity House, an intensive, in-house men’s recovery home
- Giving the residents the opportunity to model and practice new skills to replace old behaviors
- His life as a competitive athlete and sports psychology coach
- Getting the opportunity to hit the reset button
- Taking Carl Young’s advice to find the courage to look at the dark things and find freedom
- Learning to value himself enough to take care of himself
- Applying SMART tools to behaviors like over-eating or spending
- Understanding labels
- Freedom from judgement
- His perspective on Medication Assisted Treatment (MAT)
- Helping people see their value
- Finding a new hobby every year
Additional resources:
Click here to find all of SMART Recovery’s podcasts
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!

“The only way to support a revolution is to make your own” – Abbie Hoffman
The title of the post is a thinly veiled reference to the late social activist Abbie Hoffman. It has been said that the best way to get stuff done is to not have to take credit for it. The intent in posting this is to ask readers to review the ideas, take them to add to efforts to get ideas out there into the world for consideration in a spirit of contribution.
Readers may really like the ideas, readers may like some and not all, or some may not even like any of them. To all I say wonderful! Use what you like and dispense with the rest. Take in whole, modify, or even delete and move on. Feedback welcomed – I am genuinely interested in your thoughts.
So below and ATTACHED are ideas for improving our substance use care system. As Abbie said, start your own revolution, but perhaps we may all also listen to each other and seek the common ground that will benefit all of us and avoid the toxic ego centered debates that result in a quagmire of conflict that ultimately harms us all.
While largely mine in authorship, the ideas are the culmination of a whole lot of conversations with people here in PA and beyond and influenced by some of our community’s deepest thinkers.
Guiding Principles of Consideration on Treatment & Recovery for the Biden Administration
Scope of the Problem – Addiction and its consequences are arguable our greatest domestic challenges, costing lives, breaking up families with devastating community and economic consequences across our entire society.
- The COVID-19 pandemic is exacerbating the dynamics of deaths of despair and will eventually eclipse it.
- Historically, our treatment & recovery has been acute focused and fragmented. Stigma against persons experiencing addiction has resulted in a care system built on low expectations of recovery. Even the concept of abstinence as defined as not use addictive drugs in ways not prescribed has been stigmatized by some.
- Despite the reality that 85% of persons who sustain recovery over five years remain in recovery for the rest of their lives, our care system is not designed around this overarching goal.
The Goal – Our entire social service and behavioral health system should be aligned towards a long-term recovery orientation to focus on restoring individuals, families and communities to full functioning and freedom from addiction.
Treatment and Recovery Support Services – Addiction is a bio-psycho-social-spiritual disorder impacting diverse communities. We need to equitably address all aspects of it and not solely focus on biological and medical dimensions.[1]
- We believe in and support the NIDA Principles of Effective Treatment[2]. Federal funding should follow these principles and guide who and what is funded in an equitable manner that meets actual needs.
- The five-year recovery model currently only used in professional monitoring programs, should be scaled and modified to be available to everyone with an addiction, to replicate these remarkable recovery rates for persons using MAT and non-MAT pathways in order to expand recovery opportunities for millions of Americans.[3]
- Care must address polysubstance use and not be single drug focused as this is how addiction occurs in real life.
- Study and implement Cascade of Care for OUD as a framework to bridge the divide between harm reduction, prevention, treatment, and recovery and effectively build out a comprehensive continuum of care for everyone.[4]
- Full implementation and enforcement of parity for addiction treatment with other chronic conditions is essential.
Many Paths to Recovery – Recovery is a voluntarily maintained lifestyle characterized by sobriety, personal health and citizenship[5].
- People should receive individualized care. No single pathway is best for everyone.
- There is robust evidence to support Twelve Step Facilitation[6] and federal funding should be available to programs that utilize this as their treatment modality as well as other effective strategies including and beyond medication.
- Recovery builds resiliency to overcome trauma and as a result, we get better than well7.
Recovery in Criminal Justice While we must work towards getting people help prior to involvement with the criminal justice system, we recognize that this doesn’t always happen. As a result, addiction care should be provided before, during and after involvement with the criminal justice system, including pre-arrest diversion programs.8 9
Education & Workforce – All helping professionals must receive mandatory education on addiction care and recovery.
- The addiction professional workforce has a special skill set that needs to be recognized as a specialty with compensation to match10
- National credentialing standards need to be created by and for the addiction professionals they will guide.
Research – Published research should consider “real world” conditions such as polysubstance use and longer-term outcome measures focused on the bio-psycho-social-spiritual aspects of addiction and recovery.
Payment Reform – We need to incentivize long-term recovery and move away from our historically acute, fragmented care that yields poor outcomes such as continuum of care models such as the Addiction Recovery Medical Home Alternative Payment Model (ARMH-APM)11
[1] https://www.asam.org/asam-criteria/about
[2] NIDA. 2020, September 18. Principles of Effective Treatment. Retrieved from https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/principles-effective-treatment on 2020, December 3
[3] Dupont, R. L., Compton, W. M., & McLellan, A. T. (2015). Five-year recovery: A new standard for assessing the effectiveness of substance use disorder treatment. Journal of Substance Abuse Treatment, 58, 1-5.
[4] https://www.drugabuse.gov/news-events/news-releases/2019/01/cascade-of-care-model-recommended-for-opioid-crisis
[5] Betty Ford Institute Consensus Panel. What is recovery? A working definition from the Betty Ford Institute. J Subst Abuse Treat. 2007 Oct;33(3):221-8. doi: 10.1016/j.jsat.2007.06.001. PMID: 17889294.
6 Kelly JF, Humphreys K, Ferri M. Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database of Systematic Reviews 2020, Issue 3. Art. No.: CD012880Hibbert LJ,
7 Best DW. Assessing recovery and functioning in former problem drinkers at different stages of their recovery journeys. Drug Alcohol Rev. 2011 Jan;30(1):12-20. doi: 10.1111/j.1465-3362.2010.00190.x. PMID: 21219492.
8 Butzin CA, Martin SS, Inciardi JA. Evaluating component effects of a prison-based treatment continuum. J Subst Abuse Treat. 2002 Mar;22(2):63-9. doi: 10.1016/s0740-5472(01)00216-1. PMID: 11932131.
9 https://ptaccollaborative.org/about/
10 https://aspe.hhs.gov/pdf-report/substance-use-disorder-workforce-issue-brief
11 https://www.incentivizerecovery.org/

When the subject of residential treatment comes up in the addiction treatment field, there is a response I hear often (but not always). It’s a frustrating refrain. It goes like this: ‘there’s no evidence that rehab works.’
This view can and should be challenged, but what is true is that complex interventions like residential rehabilitation for drug and alcohol problems are difficult to study, say in comparison to a medication intervention. The evidence base needs to grow.
Commentators have been calling for more research for at least a decade and a half. While it’s fair to say we could do with knowing more about residential treatment, there is evidence around already. It could do with having a higher profile.
Effective Interventions

The Scottish Government have looked at this three times over the last sixteen or so years. Firstly, in 2004 the Effective Interventions Unit (EIU, now disbanded) published a paper reviewing detoxification and rehab services. Residential detoxification and rehabilitation services for drug users: A review.
The EIU found that the elements influencing effectiveness were – time in treatment, retention in treatment, client characteristics, and the provision of community aftercare. They said treatment should be at least three months long.
The authors made a recommendation: ‘Further research in this area may focus on undertaking a more detailed mapping of residential services in Scotland, improving retention rates and investigating models of good pathways of care between community and residential services.’ That mapping, it turns out, would be a long time coming.
Research for Recovery
In 2010, the Scottish Government published a paper ‘Research for Recovery’ which reviewed the evidence base. What did the researchers have to say?
‘Residential rehabilitation programmes are one of the longest established forms of treatment for drug addiction. Studies from the UK and the USA have shown improved outcomes after treatment in residential rehabilitation programmes. In DATOS, drug use outcomes after one year were good for clients who were treated in long-term residential and short-term inpatient treatment modalities in the USA.’
They also found that: ‘Regular cocaine use…was reduced to about one-third of intake levels among clients from both the long-term and short-term residential programmes, as was regular use of heroin.
In terms of opiates and harm reduction: ‘Rates of abstinence from illicit drugs have also been found to improve after residential treatment. In the UK, NTORS found that 51% of the drug misusers from residential rehabilitation programmes had been abstinent from heroin and other opiates throughout the three months prior to 2-year follow-up: rates of drug injection were also halved, and rates of needle sharing were reduced to less than a third of intake levels.’
Treatment in Scotland
In the Scottish treatment outcome study, DORIS, undertaken between 2001 and 2004, low rates of sustained abstinence were reported from stabilisation-focused community treatment. While abstinence is not necessarily the goal of medication assisted treatment, it is the goal of some seeking help for opiate problems.
What the DORIS researchers did find was that ‘residential rehabilitation treatment is more effective in promoting abstinence thirty-three months on [from the start of treatment] than other treatments outside prison. Ex-residential rehab clients were twice as likely as those who had undergone different treatments at baseline to be abstinent – apart from cannabis.’
Therapeutic communities
In our mapping of residential treatment services in Scotland, the majority of those responding reported using a therapeutic community model of treatment. A review of the published literature (from 2000) on therapeutic communities (TCs) in 2014 found: ‘TCs are generally effective as a treatment intervention, with reductions in substance-use and criminal activity, and increased improvement in mental health and social engagement evident in a number of studies reviewed.
The researchers also commented that the research ‘suggests individuals with severe substance-use disorders, mental health issues, forensic involvement and trauma histories, will benefit from TC treatment.’
2017 Review
Sheffield Hallam University published a review of Residential Treatment services in 2017. They found:
‘There is a strong and consistent evidence base supportive of the benefits of residential treatment that derives both from treatment outcome studies and randomised trials. Although more expensive, there is evidence that the initial costs of residential treatment are to a large extent offset by reductions in subsequent healthcare and criminal justice costs.
There is a clear dose effect for residential treatment with longer duration of treatment and treatment completion both strong predictors of better outcomes. A much stronger evidence base exists around attaining employment, stable housing, and ongoing support and aftercare as predictors of success.’
But treatment doesn’t stand alone:
‘There is a strong supportive evidence base around continuity of care, whether this takes the form of recovery housing or ongoing involvement in mutual aid groups.’
Their bottom line:
Overall, it is clear that an effective and recovery-oriented treatment system must include ready access to residential treatment for alcohol and drug users both to manage the needs of more complex populations and for those who are committed to an abstinence-based recovery journey
Residential Treatment Services Evidence Review 2017
2019 Review
A review of recent studies on residential treatment found that research was limited, but they did identify 23 studies of which 8 were rated as methodologically strong (including our study of a cohort of patients from Scotland). They found that the results of their research provided moderate quality evidence for the effectiveness of residential treatment in improving outcomes across a number of substance use and life domains.
They also said there is also some evidence that treatment may have a positive effect on social and offending outcomes, concluding with caution, that results suggest that best practice rehabilitation treatment integrates mental health treatment and provides continuity of care post-discharge.
2020 Working Group
Following in the footsteps of the 2004 EIU report on residential services and the 2020 review of the evidence for recovery, new work commissioned by the Scottish Government has just been completed. It was already clear that access to rehab was patchy and funding complex. The principle that residential rehab should be available to those Scots who need it was the starting point set by government. It may have taken 14 years for Scotland to answer that EIU call to map residential treatment services, but we’ve just done it and you can find a summary of what we found here. Our group also found evidence for the effectiveness of residential treatment.
Research please
As I’ve indicated, everybody who has looked at this has said the same thing – we need more research! Getting methodologically rigorous studies up and running to improve our knowledge is important. Indeed, the Residential Rehabilitation Working Group called for more research earlier this month in our recommendations.
In the service I work in, although we published one year outcomes, we now have data to five years after treatment in a cohort of patients we have been following up. Five years follow up in addiction treatment is not common!
It’s been a challenge to get resources to get the data published though I am hopeful this might change this coming year. We need long term outcome data particularly to evidence economic impacts and value for money.
Moving forward
Although we have questions about residential treatment that remain unanswered, there is already a body of evidence for its effectiveness and a commitment from the Scottish Government to make rehab more accessible. The recommendations of our group have been welcomed which is good news and we are currently developing a good practice guide. There are signs that more work may be commissioned.
Despite all I’ve written, it is important for us to remember that in terms of recovery journeys, rehab if accessed, will play a relatively small part. There is a lot of truth in the observation, that if recovery is the journey from Edinburgh to London on the train, detox is equivalent to calling the taxi and rehab is the taxi ride to the station. While there is much focus on the telephone call and that taxi journey, the largest part of recovery takes place in communities with support of mutual aid, families and community recovery resources.
That said, a significant number of people in Scotland in recovery today will acknowledge the key role rehab has played in their journey and will support efforts to make it more accessible – not in opposition to other interventions, but as well as other interventions.
I hope in 2021 that there will be more of an appetite to explore what part residential treatment should play in Scotland and that the response, ‘there’s no evidence that it works’ will be heard less and less – because it is simply not true.
Photo credit: allesandrobiascioli/istockphoto.com (under license)