Why consider the change process, and what is the application of the ideas I will present?
- Clinical addiction professionals are trained in sequential change (Stages of Change, 12 Steps, etc.) rather than continuously wholistic, organic and dynamic change processes.
- Should we always assume and work within a staged approach?
- Clinical addiction professionals are trained in symptom reduction (drug use, craving management, managing triggers, drug refusal, etc.) and personal goal attainment (gaining employment, entering school, etc.).
- Should we only work in logical steps toward attainment of concrete goals?
- Clinical addiction professionals are trained in interviewing strategies that are targeted to bring about clinically-derived outcomes, goals, and changes.
- Should we overly-rely on questions, reflections and paraphrasing meant to bring about changes chosen by the counselor?
Could it be helpful to adopt a holistically-centered method with some individuals, rather than a method centered within fixed stages, concrete steps, and questions moving toward the counselor’s goals?
A 3-sided continuous process
In recent years I became interested in experiential and phenomenological topics. For me it was time for a change. My academic training in the 1980’s was rooted in models far from the experiential and phenomenological:
- radical behaviorism
- clinical behavior therapy
- cognitive therapy
- behavioral learning models of addiction (e.g. based on Pavlovian conditioning),
- and behavior modification methods for substance problems (e.g. controlled drinking).
And I had a resulting and rather limited range of clinical experiences over a fairly long period of time.
Exploring other sources, I found a body of academic and clinical research literature that was quite different, and focused on:
- themes and patterns of change
- dynamic change processes
- synergistic processes
- tension-release, both within a person and between a person and society, and
- critical thresholds that evoke change processes and movement.
Given my background in linear models (e.g. behaviorism, cognitive-behavioral psychology) and the length of time devoted to using my original training toward rather rigorous fidelity, I was ready for something new.
In this newer learning, I was especially intrigued by one article (Jorquez, 1983) in particular, because of two key factors related to change processes that were highlighted in that paper: extrication and accommodation.
- One factor Jorquez described as critical in the change process was extrication from addiction illness and the related context and lifestyle. Being extricated from the rubble of the past made sense to me. The idea of extrication seemed natural based on my clinical experience, and additional thoughts about change I was formulating.
- Jorquez identified a second key factor in the change process: accommodation of the new. After further reading on dynamic change, I found that the basic idea of accommodation is central to change overall. And it turned out that accommodation was natural for me to consider after all, given my academic familiarity with cognitive schema and social psychology.
After considering “extrication” and “accommodation”, I took the liberty of adding “shedding” to the ideas presented by Jorquez. I meant for “shedding” to hint at things like releasing and renouncing, especially as one moves through life seasons, and reconsiders life layers.
A Visual Diagram
I decided to represent the change process that happens during clinical work, as I had it in mind, with a four-sided gem (3 sides and a base).
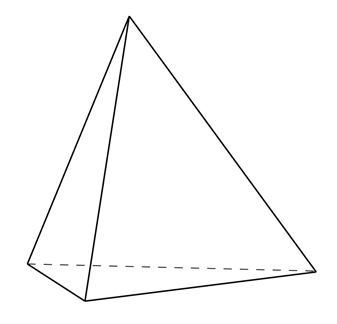 Artwork: B. Schlosser
Artwork: B. Schlosser
The top 3 sides of the gem (as adapted from Jorquez) were:
- Extrication (from)
- Shedding (the old)
- Accommodation (the new)
And in my way of thinking about this, the top three sides rotate, shift, or move together. Or they are at least dynamically enacted concurrently in the moment (non-linear; see Resnicow & Page, 2008).
For me that made intuitive sense. And it fit over three decades of my clinical observations and two resulting conclusions:
- People often do not change in a linear or predictably-ordered fashion;
- People often do the work of multiple sub-processes of change (like extrication, accommodation, and shedding) simultaneously, over long periods of time1.
But what was the base of the object going to signify?
The base, or bottom, of the change process as I wanted to represent it would be the environment brought about by the clinician.
I was introduced to some articles related to the general idea of the therapeutic environment later in my career, and they hit me particularly hard – in a good way. So, my idea was of a very particular kind of clinical environment.
One article (Bion, 1967) discussed specific aspects of clinician memory and desire. The article described how a clinician could endeavor to have no memory of the patient or past sessions with the patient, intrude into the current moment. And it also described how the clinician could endeavor to have no clinically-imposed desire for the patient’s future over-ride the current moment.
- “No memory” of the patient was hard for me to accept. But the idea in the article was for the clinician to ask themselves if they are meeting with the person, or merely with their memory of the person? The point of the challenge was to direct one’s attention wholly to the person that is with the counselor in the now, rather than the remembered version of the same person as they were in previous meetings. That kind of push for deep empathic attunement held a lot of appeal to me.
I quickly added one more feature of the clinical space I was building: “no time”.
- That might sound strange. I’ll put it like this: since starting clinical work in 1988 I have never had a clock in my office. Why is that? When the patient sits down, I endeavor for time and the keeping track of time to go away. (Admittedly, working in residential settings my whole career and long-term residential for 19 of those years fed that freedom).
I also wanted “no question asking” to be included.
- During the Behavioral Health Recovery Management (BHRM) project our leadership team decided that the Achille’s Heel of addiction counseling is the over-reliance on asking questions. Across our entire agency at that time, we endeavored to mindfully eliminate as much question asking as possible, even while conducting assessments.
Thus, in my thinking on clinical environment, “no question answering” would also be a natural stretch-goal, in keeping with basic person-centered and motivational-enhancement methods.
Lastly, given my other recent reading in philosophy, I decided demands in science, philosophical assumptions, and forced applications of clinical art were all subject to “go away”.
Expanding on Bion with my additions, I developed my personal definition of what is otherwise called “the analytic stance”. And I decided to use my formulation of the analytic stance as the base:
- No time
- No art
- No science
- No philosophy
- No question asking
- No question answering
- No memory
- No desire
Adapted from: Bion, W. (1967)
A challenge
When I introduced my formulation of the analytic stance to a workplace colleague, and explained its use in this context, I was challenged to replace it with the therapeutic “common factors” (as they are called in clinical parlance). But I declined. Why did I decline?
I knew all too well from my relatively rigid fidelity-based past that the common factors of warmth, attunement, pacing and other behaviors that can be reliably observed and scored by trained 3rd party (rating) clinicians can be feigned while fidelity is met.
Using the “common factors” was not enough.
For my newer formulation of the change process the “analytic stance” as I defined it is my preferred operational mode. Why? To me it holds both the interior (less observable) and exterior (more observable) aspects of the whole person of the therapist with more validity related to purpose, compared to techniques that are easier to replicate or feign, are pre-packaged, and perhaps more shallow.
Looking back
This later-career self-study consisted of many articles concerning multiple models of recovery from addiction illness, 12 step facilitation as a clinical practice, the mechanisms of change in 12 step recovery (in both the treated population, and untreated population), and the history and development of the concept of addiction recovery as it applies to clinical therapy and related research. And it led to additional readings. It turned out that in doing that reading I came across some remarkably interesting notions about how some change happens for some people. And those notions were not of the kind I was accustomed to.
Acknowledgments: Thanks to Katherine Mace and to Jason Schwartz for their comments on earlier drafts of this blog.
References
Bion, W. (1967). Notes on Memory and Desire. The Psychoanalytic Forum. 2:272-273, 279-280.
Jorquez, J. (1983). The Retirement Phase of Heroin Using Careers. Journal of Drug Issues. 13:343-365.
Resnicow, K. & Page, S. E. (2008). Embracing Chaos and Complexity: A Quantum Change for Public Health. American Journal of Public Health. 98(8):1382-1389.
Suggested Reading
1 Here we have a research observation that people undergoing addiction treatment might be simultaneously brainstorming hoped-for possible selves to pursue, feared possible-selves to avoid, refining and narrowing those choices over time, and developing and revising related action strategies – all while roughly progressing through Stages of Change relative to their SUD. Dunkle, C., Kelts, D. & Coon, B. (2006). Possible Selves as Mechanisms of Change in Therapy, in C. Dunkle & J. Kerpelman (Eds.) Possible Selves: Theory, Research and Application. (pp. 186-204). Nova Publishers.
Marquis, A., Douthit, K. Z. & Elliot, A. J. (2011). Best Practices: A Critical Yet Inclusive Vision for the Counseling Profession. Journal of Counseling & Development. 89: 397-405.
Thomas, C. (2013). Ten Lessons in Theory: An Introduction to Theoretical Writing. Bloomsbury Academic: New York.
White, W. L. (2007). Addiction Recovery: Its Definition and Conceptual Boundaries. Journal of Substance Abuse Treatment. 33: 229-241.
In celebration of National Recovery Month, Fellowship Hall will be highlighting the stories of some of our incredibly inspiring alumni and staff members on social media and here on our blog. It is our hope that in sharing these stories, we break the stigma surrounding drug and alcohol addiction. With knowledge, we can advocate for the proper treatment of ourselves and loved ones that may struggle with the disease.
***
There’s an old saying that goes, “No matter where life takes you, don’t forget where you came from,” and Fellowship Hall staff member Christina T’s story is an incredible reminder of the truth behind this cliché.
The year was 2008, and Christina had been recently released from her third stint in prison. As she returned to life beyond confinement, she began to seek employment  through Graham Temporary Services. Whether it was by coincidence or true fate, she was offered a job at Fellowship Hall as the head of housekeeping. At the time, she had no way of knowing that this facility would go on to have such a major impact on her life and career path. As Christina settled into her work and daily routines, things began to look up. However, life happens, and unfortunately—so do relapses. Christina would go on to relapse once more and spend a final time in prison from 2009 – 2011.
through Graham Temporary Services. Whether it was by coincidence or true fate, she was offered a job at Fellowship Hall as the head of housekeeping. At the time, she had no way of knowing that this facility would go on to have such a major impact on her life and career path. As Christina settled into her work and daily routines, things began to look up. However, life happens, and unfortunately—so do relapses. Christina would go on to relapse once more and spend a final time in prison from 2009 – 2011.
After her final release in 2011, Christina had a plan—her sights were set on getting back to the place that had once provided her with a sense of structure and purpose. “I came back to what I knew. I came back to Fellowship Hall to ask for a job again,” Christina explained.
At the time, no positions were available, but thankfully, she was unwilling to give up on another chance to work at the Hall. “I just wanted to be here [Fellowship Hall] and I was not going to give up,” she said. For eight months, Christina kept in touch with the Hall until one day in August of 2012, she got the call she had been waiting on—one that arguably, would change her life and allow her to begin building a future that she could be proud of. A position in the kitchen as a Dietary Aid (which she described as “a fancy title for a pot washer”) was open. Nevertheless, she gratefully accepted. Her first day back at work was also her first day back to school.
Christina enrolled herself in classes at Guilford Technical Community College to study for an Associate Degree in Human Services. After a year and a half in the program, she decided to go all the way in pursuit of a Bachelor’s Degree. She applied twice to UNCG and once to A&T but was denied all three times. Once again, Christina had the tenacity to not give up.
She researched other opportunities to get her education and was accepted to the Western New Mexico University School of Social Work online program. She earned not only a Bachelor of Social Work in May of 2017, but continued on and earned a Master of Social Work in May 2018. Currently, she is in the process of acquiring her LCAS and LCSW-A License.
As the doors to education were opening for Christina, new job opportunities presented themselves at the Hall as well. She moved from the kitchen to work as a part-time therapy assistant and a part-time receptionist. Finally, in 2015, she was offered a full-time position with Admissions. When potential guests call admissions, they establish the first point of contact with Fellowship Hall. Often, they are reluctant, nervous, and scared—sometimes they’re only calling because they have been forced to seek treatment. Through her own experience and education, Christina was able to provide the guidance and compassion that the individuals deserved. She found her work with admissions to be genuinely rewarding and said that her then supervisor, Randy Carter, supported her tremendously for three years as an admission counselor while she was both working and in school full time.
In 2018, Christina transitioned from Admissions to Therapy as a Social Assessment Counselor, in which she performed in-depth social assessments for guests and helped to build their treatment plans. Christina now serves as a Primary Counselor for those in treatment. As Fellowship Hall admires her persistence, strength, and dedication to treatment, Christina acknowledges the support that afforded her the opportunities she is able to exercise today.
“Everyone at Fellowship Hall has been so supportive, including the board who approved my education reimbursement, HR has supported my changes in positions, and Kelly [Scaggs, Clinical Director] gave me the opportunity to join the clinical team and has been very supportive of my professional growth. It’s a privilege I have been given to use my experience and education to help others suffering from addiction find their own journey. I love Fellowship Hall. I believe in what we do and I believe we do it well.” Christina is now officially a Licensed Clinical Addiction Specialist and Licensed Clinical Social Worker Associate.
Something that makes Fellowship Hall so unique in the realm of treatment facilities is the staff. Like Christina, many of our well-trained, highly qualified staff are in recovery themselves and have seen the trials and tribulations of rebuilding a life after active addiction. It is not uncommon to hear from Alumni that building relationships with staff such as Christina, gives them the motivation and confidence to actively pursue a life in recovery.
For more information, resources, and encouragement, ‘like’ the Fellowship Hall Facebook page and follow us on Instagram at @FellowshipHallNC.
About Fellowship Hall
Fellowship Hall is a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers. We are committed to providing exceptional, compassionate care to every individual we serve.
This piece, entitled “Britain has to overhaul its attitude to drug use – moralising isn’t the solution,” popped up in my email and more than once in my twitter feed.
Various versions of this argument are very common in drug policy circles, and I’d suggest (again) that it’s the wrong direction to try to take the discussion.
First, you might think it strange if you came to a friend with a problem and their approach was to remove your values and moral beliefs from the equation. It might be necessary to reveal hidden values/moral, examine them, explore the tensions between them, challenge them, and possibly replace them with different values. But, to eliminate them from decisions of great consequence? That’s a bad strategy. (Unless you really believe, like Sam Harris, that science can answer all moral questions.)
Second, the author equates moralizing with vilification, snobbishness, looking down upon others, racism, an absence of sympathy, the targeting of oppressed groups, scolding, shaming, stigma, criminalization, prudishness, and finger-wagging.
Third, I’d suggest that the author is engaged in their own version of moralizing–rejecting one set of values and calling for another. Calls for drug policy reform are invariably moral arguments, even when they reject morality as an element of policy formulation.
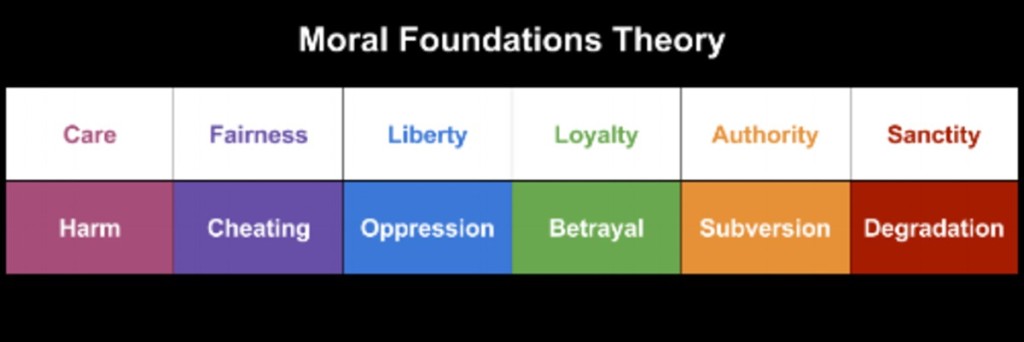
I’d suggest that the best response to the misapplication of morals, or the application of the wrong morals is not to eliminate morals from decision-making. The better way would be to examine and clarify the values/morals involved. It may be that we believe current policies overemphasize sanctity and authority, and undervalue care and fairness. (Moral Foundations Theory is only one way to examine this. Obviously, it’s not the only way.)
So, I’m suggesting that the problem isn’t moralizing in drug policy, it’s that we need to interrogate our value/moral hierarchy.
Further, I believe that pretending some approaches are value-free makes that task more difficult.
Finally, as I’ve said many times in this blog, there is no such thing as a problem-free drug policy, there are always going to be trade-offs. This means that any honest examination of our options means choosing which problems we’re unwilling to live with, and which problems we’re willing to tolerate.
Even then, our ability to will these choices into reality is limited–we have influence but not control.
Something went awry with yesterday’s post, so I’m reposting and adding a video shared in a comment.
This interview with Keith Humphreys is well worth the time, particularly if you don’t have first hand experience with 12 step recovery.
For more info, visit David McCartney’s post on the Cochrane Review discussed in this interview.
Here’s a video from the Recovery Research Institute on the same topic.
This interview with Keith Humphreys is well worth the time, particularly if you don’t have first hand experience with 12 step recovery.
For more info, visit David McCartney’s post on the Cochrane Review discussed in this interview.
Alexander Cardé wants to shout from the rooftop so that everyone would know about SMART Recovery. Instead he uses his passion and voice to facilitate face-to-face and online meetings. He encourages people to take the Get SMART Fast Training Program because he knows SMART makes an impact in people’s lives, just like it did in his.
View the full video on our YouTube channel
Read more about becoming a SMART Volunteer
Subscribe to the SMART Recovery YouTube Channel
Video storytelling is a powerful tool in recovery, and we are proud to share our SMART Recovery content free-of-charge, available anywhere, on any device. Our videos inform, entertain, and inspire.
Subscribe to our YouTube channel and click on the Notifications Bell to be alerted every time we release a new video.
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
Written by SMART Family & Friends Facilitator, Kathy Lang

In the online Family & Friends meetings that I facilitate, one of the more difficult issues that sometimes arises is the decision whether to end a relationship with a family member struggling with addictive behavior. Faced with the frustration, exhaustion, and negative emotions that have developed, many people reach a place of hopelessness before coming to a meeting.
New participants are encouraged to learn that our approach, which uses evidence-based methods, is very different than what they are familiar with. Generally they have heard the wider cultural norm of “kick them to the curb” and “let them hit rock bottom.” When participants hear the experiences of others practicing the SMART tools, they typically feel some relief that they may be able to do something to help themselves and resuscitate the relationship with their loved one.
What I often say in this situation is that the “When to Quit?” worksheet in our handbook is placed very near the end of the book for a reason. Newcomers are usually responsive to the idea of postponing any decision and giving the SMART approach a try.
So what do they learn from attending our SMART meetings and using our handbook? They learn to give up the role of fixer, coming to the realization that they cannot force their loved one to choose recovery. In our meeting we often use a quote from the book Beyond Addiction: How Science and Kindness Help People Change:
“Everything we know about motivation and change suggests that power and powerlessness come with the territory of caring about someone with a substance problem.You have the power to help someone change, and the power to make changes yourself that will improve your situation, yet you are powerless to make another person change or do the changing for him.”
Participants learn to better understand boundaries and the importance of developing and maintaining them. They develop better communication skills through using the P-I-U-S approach. They gain skill in managing their emotions more effectively through the use of cognitive tools like the ABC, Anti-Awfulizing, the FEAR Exercise, and knowledge about the stages of change and facts about addiction. Critically important, they learn to practice self-care with two goals: understanding that they can survive and thrive regardless of the choices of their loved one and understanding that they cannot effectively support their loved one with depleted physical and emotional resources (we use the analogy of the oxygen mask on an airplane that instructs us to put our mask on before assisting others).
However, despite a family or friend’s best efforts, they sometimes reach a point of questioning whether they can continue in a relationship when their loved one has shown no motivation to give up the addiction. Often dealing with serious consequences to themselves and other family members (especially when there are children in the home), they struggle with balancing self-protection needs and their desire to maintain a supportive relationship with their loved one.
That’s when the exercise “When to Quit?” in our handbook is useful. If the family or friend has successfully practiced newly learned skills for a period of time, without movement of their loved one toward recovery, then they may decide to choose end the relationship.
Sometimes this decision brings feelings of guilt. SMART tools can help with the process of ending the relationship. Having reached a place of better understanding of addiction and greater empathy for their loved one, a participant can face this ending with more compassion and less anger. Although they can no longer see a future in the current relationship, they can part with a recognition that blame will not help the situation – not blaming their loved one or themselves. They can leave the relationship knowing they have done their best, with kindness towards their loved one, recognizing the worth of their loved one and the past value of their relationship. In doing so they demonstrate the importance of what they have been working to accomplish – not allowing what they cannot do stop them from doing what they can. In addition they take the tools they’ve learned to enhance an emotionally healthy life for themselves as their future unfolds.
About SMART Recovery Family & Friends
SMART Recovery Family & Friends helps those who are affected by substance abuse, drug abuse, alcohol abuse, or other addictions of a loved one. Our program is a science-based, secular alternative to Al-Anon and the Johnson Intervention, and our method is based on the tools of SMART Recovery and CRAFT (Community Reinforcement and Family Training). CRAFT aims to teach family and friends self-protection and non-confrontational communication skills to help their addicted loved one find recovery.
You can find Family & Friends meetings in-person and online.
If you are interested in starting a Family & Friends meeting in your local area, we would love to hear from you. Please click here to learn more about starting a Family & Friends meeting.
Click here to read more about SMART Recovery Family & Friends.
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.
You have Successfully Subscribed!
How to Lend a Hand to Someone in Need of Recovery
Every September, the Substance Abuse and Mental Health Services Administration (SAMHSA) sponsors Recovery Month to increase awareness and understanding of mental and substance use disorders and celebrate those in recovery (www.recoverymonth.gov).
At Fellowship Hall, we work to dispel the stigma surrounding substance use disorder: no one is immune to this disease. It impacts those using, as well as friends and loved ones and can be incredibly daunting and confusing to navigate.
Do you have a loved one or friend struggling with Substance Use Disorder? Here are 4 things you can do to help:
GET EDUCATED
The most empowering thing that you can do is to educate yourself about the disease. There’s endless resources on www.aa.org, www.na.org, and support specifically for friends and loved ones on www.al-anon.org, www.nar-anon.org The more you know about the disease, the better you can support someone who is struggling. If someone you love is in active danger or in a situation that you believe to be a medical emergency, call 911 immediately before proceeding.
PRACTICE EMPATHY
Being empathetic is achievable without being an enabler. The disease often drives individuals to do things incredibly out of character. Your loved one may be lying to you, lashing out, and making your life feel overall unmanageable. During these times, demonstrating empathy may be the last thing you want to do, however, it is one of the most tactful ways to encourage your loved one to seek treatment while preserving your own sanity. Substance use disorder changes our loved ones, and addressing these changes is necessary to their health and safety as well as our own.
Being empathetic includes:
- Avoiding judgement
- Avoiding criticisms
- Addressing issues in a non-confrontational way
- Showing concern
- Providing solutions without pushing
- Meeting them with love and compassion
PRACTICE SELF-CARE AND SET BOUNDARIES
You cannot help someone else get better if you aren’t taking care of your own personal well-being first. Caring for or loving someone suffering from substance use disorder can be taxing on our physical, emotional, and mental health. Utilize support networks such as Al-Anon or Nar-Anon. Talk to a counselor or professional about what you’re going through, and prioritize your health first. Remember, you are not responsible for your loved one’s disease. Set boundaries with this individual and yourself. Make them aware of said boundaries, and hold them accountable. Boundaries can include:
- Not allowing them to be in your space if they are drinking or using
- Walking away from a conversation that becomes argumentative
- Not giving the individual money
COMMUNICATE EFFECTIVELY
If it were as easy as telling someone to “go get help,” no one would suffer from substance use disorder. The individual has to accept that they are sick and want to get better before treatment can be effective. This is not something you can force anyone into doing. Denial will protect them from realizing that they are sick or that they need help. You can only try to lead them to acceptance with effective communication. This may include:
- Asking questions that encourage open conversation and reflection instead of making statements that may come across as accusatory.
- Communicate the way the individual’s actions make you feel with stern compassion. This means you are owning your own individual feelings, while making sure that they know you will not tolerate actions or words that cross your personal set boundaries.
- Make sure the individual knows that you are willing to help them seek proper treatment and eager to support them in doing so.
Ultimately, you must remember that you cannot control those in need of treatment, in most circumstances, you can only encourage them to seek proper treatment. Be strong and be patient. For the sick individual, getting well can be a long and arduous process, but it will be one of the most rewarding things they ever do for themselves. If your loved one is interested in seeking treatment at Fellowship Hall, please visit https://www.fellowshiphall.com/admissions.php
At Fellowship Hall, our mission is to help those struggling with substance use disorder by providing compassionate, cost-effective care. For more information, resources, and encouragement, ‘like’ the Fellowship Hall Facebook page and follow us on Instagram at @FellowshipHallNC.
About Fellowship Hall
Fellowship Hall is a 99-bed, private, not-for-profit alcohol and drug treatment center located on 120 tranquil acres in Greensboro, N.C. We provide treatment and evidence-based programs built upon the Twelve-Step model of recovery. We have been accredited by The Joint Commission since 1974 as a specialty hospital and are a member of the National Association of Addiction Treatment Providers.

It is an age-old story, out of area well-meaning experts descend on a community bearing big ideas, big money and big projects to improve things for the natives. They build a road, dam, or a well or a school and fundamentally change the dynamics of things that were working in those communities before their arrival. As they are experts, they do not ask the locals what their needs are, how they may assist the local communities to strengthen what is already in place or even how to complete projects in ways that strengthen the local infrastructure or workforce over the long term.
The project may actually improve functioning within the community in the short term. But the local resources end up withering away as the new project meets some need. In other instances, the project has no real use of the community as it was something that we developed and implemented without community input. Some of the projects may be what are called white elephants, and the upkeep of them takes resources away from some other local need and further erode the functioning of the community. Either way, there is great fanfare for the projects and the out of area experts congratulate themselves on the great things that they have done for the locals.
As there was a lack of engagement with the community, the projects inadvertently fostered dependency and were not developed in ways that leveraged and strengthened these communities. The community begins to rely on the school or the dam or the well for their community needs and abandon how they did it before the experts came, forgetting lived experience. The locals are no longer autonomous, they are in a dependency role, reliant on the out of town experts and their projects.
No local knowledge or local capacity is expanded. This is perhaps because it seemed easier for the out of town experts to do it themselves, or perhaps the money was seen as better spent internally between the experts and not externally within the community. Or perhaps they even looked down on the locals, believing that their ways were better and the locals not properly enlightened.
Sooner or later the money dries up and the well-meaning experts roll out of town as quickly as they arrived. As there had been no real engagement with the local people on these projects, the projects begin to deteriorate. As the communities have begun to rely on these projects for their needs, the things that they were doing before the arrival of the out of town experts is no longer in place. Resources that had been used to support other needs in the community before the arrival of the out of town experts are further diverted to support the white elephant projects, further reducing the available resources within the community.
The projects end up failing over time and the local community no longer has either the new (and now failed) projects or the skills or infrastructure to support the way that they were meeting the need before the out of town experts had arrived. The out of town experts are long gone by this point, they are on to the next project and descending on the next group of natives. Sadly, the community ends up in worse shape than they were before the out of towners had come. The money, that could have been used to support the development of those communities in an authentic way are frittered away, the well dry, the road washed away, the school empty, the dam no longer operational and all the money long gone.
How does this relate to authentic recovery communities, all the federal money coming down to the state across the nation and why we have our basic ethos of “nothing about us without us?”
Perhaps you can tell me.

In the United States Army, he was an E-4 Specialist with the 42 INF Div., serving in Guantanamo Bay, Cuba. As a private person, Michael Hooper was a man struggling with alcohol abuse and depression. He didn’t know where to get help until he called the Veteran’s Crisis Hotline. From there Michael was introduced to SMART Recovery through the VA Hospital. He knew from the first meeting it was “going to be a life changer,” but it wasn’t until a four-month intensive, inpatient program, that Michael realized how valuable the SMART Recovery program was for his survival.
The program was effective for Michael because there was a direct sense of purpose and self-empowerment, which resonated with his military training. After completing the facilitator training, he felt compelled to pay it forward and started facilitating his own meetings to share SMART with more people in his Hackensack, New Jersey, community.
Now, in his new role as the State Outreach Director for Ohio, Michael will bring his authenticity, passion and lived experiences to new audiences that might otherwise never hear of SMART. He says, “having grown up in a minority neighborhood, the need for non-profit services in these communities is great. The individuals suffering in these communities deserve the same opportunities as everyone else.” He hopes to get more communities involved with meetings and available resources. Michael will also continue to expand outreach within the VAs, schools, and prison systems in Ohio. This is a “boots on the ground position,” he says, that will take him where he is needed because “outreach is here to help save lives.”
Subscribe To Our Blog
Join our mailing list to receive the latest news and updates from the SMART Recovery Blog.


